If you take amlodipine for high blood pressure and you have glaucoma (or you’re at risk), you want a straight answer: is this a safe combo? Here’s the short, practical version. Amlodipine doesn’t directly raise eye pressure. The real issue is blood flow to the optic nerve-go too low on systemic blood pressure, especially at night, and glaucoma can creep forward even with decent eye pressures. You don’t need panic, you need a plan: pick sensible BP targets, monitor symptoms, time your doses wisely, and sync your GP and eye specialist.
- TL;DR: Amlodipine is usually fine in glaucoma. The risk isn’t a spike in eye pressure-it’s dropping blood pressure too low (especially overnight), which can reduce optic nerve perfusion.
- Ask for an IOP check 4-8 weeks after starting or increasing amlodipine, earlier if vision feels off.
- Extra caution if you have normal-tension glaucoma or documented progression despite good IOP-consider 24-hour ambulatory BP monitoring.
- Watch for dizziness, dimming vision, or “grey-outs” on standing-these can hint at under-perfusion.
- Tell your eye doctor all your heart/BP meds. Beta-blocker eye drops with multiple BP drugs can slow the heart too much.
What you actually want to know about amlodipine and glaucoma
Most people who click on this topic have the same jobs to be done. They want to know if they can keep their blood pressure controlled without making glaucoma worse, they want to understand any drug interactions, they want timing and monitoring tips, and they want a plan for what to do if something feels off. Let’s hit those one by one.
First, what does amlodipine do? It’s a dihydropyridine calcium channel blocker. It relaxes vascular smooth muscle so arteries open up, which drops blood pressure and reduces cardiovascular risk. No anticholinergic effects, no pupillary dilation. It doesn’t trigger angle closure. In short: it doesn’t directly push your eye pressure up.
So why the anxiety? Because glaucoma is more than an eye-pressure number. The optic nerve needs adequate perfusion pressure. If systemic blood pressure falls too low relative to your intraocular pressure (IOP), the nerve can be starved of flow. Observational research, going back to population work like the Baltimore Eye Survey, shows low ocular perfusion pressure is linked to open-angle glaucoma. More recent studies and nocturnal monitoring research report that nighttime dips in blood pressure-especially diastolic pressure-are associated with faster visual field loss in susceptible patients, even when IOP looks fine in the clinic.
That’s the core tension: treat blood pressure (good for your heart and brain) without over-treating (bad for optic nerve perfusion in some patients). For most people, the balance is straightforward: aim for guideline-range blood pressure while keeping an eye on symptoms and your eye pressures. For a subset-normal-tension glaucoma, documented progression with “good” IOP, or heavy nocturnal dipping-you and your doctors may tweak the plan.
I’ll flag the key term you were probably searching: Amlodipine and glaucoma. The short answer is that they can coexist, with sensible precautions.
Does amlodipine change intraocular pressure or glaucoma risk?
Direct IOP effect: Amlodipine doesn’t raise intraocular pressure. It’s not a steroid, it doesn’t dilate the pupil, and it doesn’t interfere with aqueous humor outflow in a meaningful way.
Indirect risk: The worry is excessive systemic blood pressure reduction, particularly overnight. Ocular perfusion pressure (OPP) is roughly two-thirds of mean arterial pressure (MAP) minus IOP. If IOP is steady but MAP drops, OPP drops. If OPP gets too low for your individual optic nerve, damage can progress.
Here’s a simple way to think about perfusion:
- Mean arterial pressure (MAP) ≈ (Systolic + 2 × Diastolic) ÷ 3.
- Ocular perfusion pressure (OPP) ≈ 2/3 × MAP − IOP.
- Lowering IOP boosts OPP; lowering systemic BP reduces OPP.
What the evidence says:
- Population studies have linked low perfusion pressure with a higher prevalence of open-angle glaucoma.
- Nocturnal hypotension studies show greater glaucoma progression in people whose diastolic BP dips more overnight.
- Some observational datasets report an association between systemic calcium channel blocker use and higher odds of glaucoma; others don’t. These are not randomized trials and are prone to confounding (people on BP meds have different vascular risk profiles).
Guideline perspective:
- Glaucoma guidelines (AAO Preferred Practice Pattern; RANZCO care statements) encourage coordination with the patient’s GP/cardiologist, especially where progression occurs with good IOP, or where symptoms suggest hypotension.
- Hypertension guidelines (e.g., 2023 European and Australian guidance) set targets but caution against pushing diastolic BP too low in older adults. Many specialists try to keep diastolic BP > 60 mmHg, especially at night, in patients with progressive normal-tension glaucoma. This is individualized-no single number fits all.
Bottom line: amlodipine itself isn’t the villain. The risk is overshooting your blood pressure target. You win by aiming for good cardiovascular control while protecting optic nerve perfusion, especially if your glaucoma has progressed despite “normal” eye pressure.
Safe-use checklist: starting, switching, and monitoring without guesswork
Use this as a practical, repeatable process whenever your blood pressure meds change.
- Before you start or increase amlodipine:
- List all eye meds and heart/BP meds. Bring it to your GP and eye specialist.
- Note your most recent IOP and visual field status.
- Know your typical home BP (if you have a monitor). Write morning and evening averages for a week.
- First 2-8 weeks after a dose change:
- Check home BP at different times: on waking, mid-afternoon, before bed. Keep a log.
- If you feel light-headed on standing, check BP sitting and then 1-3 minutes after standing. Report large drops (≥20 systolic or ≥10 diastolic).
- Ask for an IOP check 4-8 weeks after starting or increasing amlodipine-or sooner if your vision feels less crisp, you’re getting grey-outs, or morning vision seems worse.
- Timing matters (especially if you have normal-tension glaucoma):
- Consider taking amlodipine in the morning if you’re a heavy nocturnal dipper. This is not universal-check with your GP.
- If you’re on multiple BP agents, avoid stacking them all at night unless your doctor is aiming to blunt morning surges for a clear reason.
- When to ask for ambulatory BP monitoring (ABPM):
- Normal-tension glaucoma with progression despite IOP at target.
- Symptoms of nocturnal hypotension (waking with dim vision, morning headaches, fatigue) or big daytime orthostatic drops.
- Targets and guardrails (discuss with your clinicians):
- BP goals should reflect your age, comorbidities, and cardiovascular risk. Many older adults do best with systolic 120-139 if tolerated.
- Be cautious about diastolic < 60 mmHg, particularly overnight, if glaucoma is progressing.
Australian note: amlodipine is PBS-listed, widely used, and often first-line. If you’re here in Melbourne like me, your pharmacist can help check for interactions with eye drops, and Medicare covers regular eye exams-so use that safety net.

Drug interactions and mix-and-match issues with glaucoma drops
Most glaucoma eye drops are fine with amlodipine. The stand-out interactions happen when multiple heart-slowing or blood-pressure-lowering drugs stack up, including systemic effects from “just eye drops.” Here’s a fast map you can use with your clinicians:
| Glaucoma drop class | Common drugs | Main systemic effect | Interaction concern with amlodipine | Monitoring tips |
|---|---|---|---|---|
| Prostaglandin analogues | Latanoprost, Bimatoprost, Travoprost | Minimal systemic effects | None significant | Standard IOP checks |
| Beta-blockers | Timolol, Betaxolol | Lower heart rate, lower BP | Possible additive BP lowering; bradycardia risk higher if also on oral beta-blocker, verapamil, or diltiazem | Check pulse/BP; report dizziness, fatigue, near-syncope |
| Alpha-agonists | Brimonidine | Can lower BP, cause fatigue | Mild additive BP lowering possible | Watch for daytime sleepiness, low BP symptoms |
| Topical carbonic anhydrase inhibitors | Dorzolamide, Brinzolamide | Minimal systemic effect | No meaningful interaction | Standard monitoring |
| Oral carbonic anhydrase inhibitor | Acetazolamide | Diuresis, electrolyte loss | May compound dizziness/low BP symptoms | Hydration, electrolytes if prolonged use |
| Rho-kinase inhibitors | Netarsudil | Minimal systemic effect | No meaningful interaction | Standard monitoring |
| Miotics | Pilocarpine | Minimal systemic effect | No meaningful interaction | Standard monitoring |
A few practical points:
- If you’re on a non-dihydropyridine calcium channel blocker (verapamil or diltiazem), be extra cautious with timolol drops-those combos can slow the heart. Amlodipine is less of a bradycardia problem but still watch for symptoms.
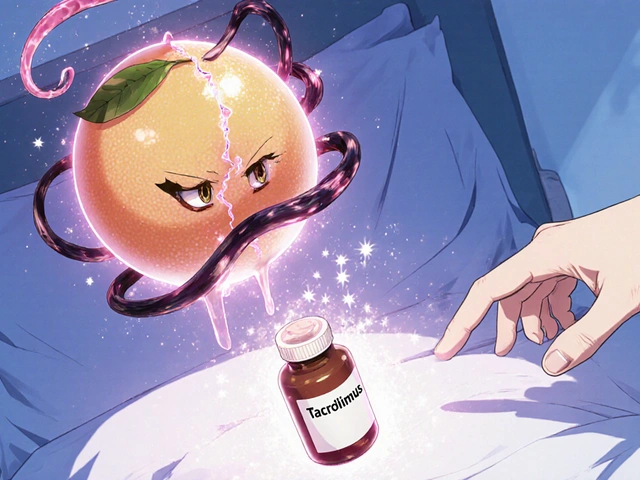
- Grapefruit juice can raise amlodipine levels. That can translate to more ankle swelling or lower BP. Not a glaucoma issue per se, but relevant if you feel woozy.
- No link between amlodipine and angle-closure glaucoma. Decongestants and strong anticholinergics are the drugs that can trigger angle closure in susceptible anatomies, not amlodipine.
Real-world scenarios, red flags, and course-corrections
Here are the patterns I see most in clinic and how to handle them.
- Scenario: You start amlodipine 5 mg. After a week, your home BP averages 122/68, you feel fine, eyes feel normal.
- Plan: Keep going. Book an IOP check in 4-8 weeks. Log BP twice a day for 7 days before that visit.
- Scenario: You’re 72 with normal-tension glaucoma. Visual field progression over the last year despite IOP 12-14 mmHg on latanoprost. Your GP increased BP meds recently; your morning home BP is 110/58.
- Plan: Share the visual field trend with your GP. Consider ABPM to see nocturnal patterns. Discuss spreading BP meds earlier in the day or modest dose reduction if safe for your heart risk. Your eye doc may also aim for even lower IOP or adjust drops.
- Scenario: On timolol drops and amlodipine, you feel sluggish, with a pulse of 52.
- Plan: Call your GP and eye specialist. It may be as simple as switching from timolol to a prostaglandin analogue or reducing systemic beta-blockade if you’re on one.
- Scenario: You notice morning “grey-outs” when you stand up.
- Plan: Check orthostatic BP at home. If drops are big, talk to your GP about dose timing or adjusting therapy. Ask your eye clinic for an earlier pressure check.
Red flags that deserve a phone call:
- New, persistent dimming or blurring of vision, especially on waking.
- Frequent light-headedness, near-fainting, or falls.
- Visual field changes you can notice (new blind spots, arcs, or “missing” patches).
- Resting heart rate persistently below 55 with fatigue or dizziness.
Simple self-check rules of thumb:
- If your diastolic BP is repeatedly in the 50s and you have glaucoma progression, ask about ABPM and dose timing.
- If your ankle swelling ramps up on amlodipine, that’s a dose/side-effect conversation-swelling doesn’t harm the optic nerve, but it tells us about your drug level.
- If your IOP goes up after a BP med change, that’s usually unrelated to the amlodipine-look for steroid exposure, drop adherence, or measurement variability.
FAQs and what to do next
Q: Does amlodipine raise eye pressure?
A: No. It doesn’t increase aqueous production or block outflow. The concern is blood pressure going too low, not IOP going too high.
Q: Is amlodipine safe with latanoprost?
A: Yes. That’s a common and safe combination.
Q: Can amlodipine cause angle-closure glaucoma?
A: No. It doesn’t dilate the pupil or have anticholinergic effects, which are the usual culprits for angle closure.
Q: I’m on timolol eye drops and feel more tired after starting amlodipine. Related?
A: Possibly additive effects on blood pressure and pulse. Check your heart rate and talk to your GP and eye doctor. A drop change often fixes it.
Q: What’s the “best” BP medicine for someone with glaucoma?
A: There isn’t a one-size-fits-all. Amlodipine, ACE inhibitors, ARBs, and thiazides can all be fine. For patients with progressive normal-tension glaucoma and nocturnal dips, morning dosing and avoiding very low diastolic pressures can matter more than the specific drug.
Q: Should I stop amlodipine if my glaucoma gets worse?
A: Don’t stop on your own. You need a coordinated plan-check eye pressures and visual field trend, review BP logs, consider ABPM, adjust dose timing, and set a realistic BP target that protects both your heart and optic nerve.
Q: Any special advice for Australia?
A: Keep using Medicare-funded eye checks, bring your PBS medication list to appointments, and ask your pharmacist to flag interactions between your heart meds and eye drops.
Next steps if you’re starting or already on amlodipine:
- Write down your current eye meds, systemic meds, and allergies.
- Record home BP for a week (morning and evening). Note any dizziness or visual dimming.
- Book an IOP check 4-8 weeks after any BP med change.
- If you have normal-tension glaucoma or unexplained progression, ask your GP about 24-hour ABPM and whether morning dosing fits your pattern.
- Share your BP log and eye clinic results across both teams-GP/cardiologist and ophthalmologist/optometrist.
When to escalate quickly:
- Severe dizziness, near-fainting, or a resting pulse in the 40s-call your GP or urgent care.
- Sudden eye pain and halos with a fixed mid-dilated pupil-this sounds like acute angle closure, which is unrelated to amlodipine but needs urgent care.
Credibility check-where this advice lines up with the literature and guidance you can trust: the American Academy of Ophthalmology Preferred Practice Pattern for Primary Open-Angle Glaucoma, RANZCO care statements, major population studies linking low ocular perfusion pressure with glaucoma, nocturnal hypotension research linking excessive nighttime dips with progression, and the Australian product information for amlodipine (TGA). Hypertension targets and cautions around very low diastolic pressure reflect 2023 hypertension guidelines used in routine care here and abroad.
You can keep your heart safe and your optic nerve protected. Most people do fine on amlodipine with a few smart guardrails: don’t overshoot BP lowering, check in after dose changes, and speak up fast if your body gives you clues-dimming, dizziness, or a visual field that doesn’t feel right.




Brian Mavigliano
When the world tells us that a calcium channel blocker automatically means safety for the optic nerve, I delight in the contrary whisper of doubt. Philosophically, every drug is a dual‑edged sword, carving pathways through arteries while carving opportunities for hidden perils. Amlodipine, with its silky vasodilatory caress, may lower systemic pressure to a level that the retinal perfusion can no longer draw life‑sustaining blood. Imagine the eye as a candle flickering in a draft; the draft is your blood pressure and the flame is the optic nerve's metabolic fire. When the draft becomes too strong, the flame sputters, even if the candle's wax (the intra‑ocular pressure) stays untouched. Clinical anecdotes abound where patients with well‑controlled IOP still witnessed field loss after aggressive nocturnal BP dips. Thus, the safety mantra that “amlodipine doesn’t raise IOP” is accurate but incomplete, like stating that a hurricane doesn’t bring rain while ignoring the flood it may cause. The art lies in calibrating the dosage so the arterial pressure hovers above the perfusion threshold, especially during the sleep‑induced troughs. Chronotherapy-shifting the dose to the morning-can rescue that nocturnal dip, a trick the literature nods to but the lay‑man rarely hears. Patients with normal‑tension glaucoma should treat their blood pressure as a variable, not a constant, and monitor orthostatic symptoms like a sailor watches the horizon. A simple home‑BP log, taken at waking, midday, and bedtime, can reveal the silent assassin that is nocturnal hypotension. If you notice dizziness, grey‑outs, or a sudden dimming of vision upon standing, those are the warning sirens of under‑perfusion. In practice, coordinating your GP and ophthalmologist to share these logs is as vital as sharing a secret code among comrades in battle. Remember, the goal is not merely to tame hypertension but to protect the optic highway from traffic jams of low pressure. So, while amlodipine may be benign to the trabecular meshwork, its systemic influence can still orchestrate a stealthy assault on vision. Choose your allies wisely, monitor vigilantly, and the combination can be as harmonious as a well‑tuned orchestra.
Emily Torbert
Sounds solid just keep an eye on any dizziness and let your doc know ASAP
Rashi Shetty
It is incumbent upon every patient to recognize that neglecting systemic blood pressure control in the presence of glaucoma would be an act of reckless self‑endangerment. Conversely, the reckless over‑correction of blood pressure, especially nocturnally, betrays a disregard for the fragile equilibrium of ocular perfusion. Both extremes betray the moral duty of stewardship over one's own health. Thus, a balanced approach, guided by regular IOP assessments and ambulatory BP monitoring, is not merely advisable but ethically obligatory. Failure to adhere to these safeguards may lead to irreversible visual loss, a tragedy that could have been averted with due diligence. ❗️👁️
Queen Flipcharts
Our great nation has long championed the integration of cardiovascular health with ocular preservation as a testament to holistic medicine. Employing amlodipine, a drug forged in the laboratories of our allies, exemplifies the patriotic choice of evidence‑based therapy. Yet, the same spirit of vigilance that protects our borders must guard the optic nerve against the silent incursions of hypotension. Strategic timing of dosage, preferably aligned with daylight hours, mirrors the disciplined cadence of our national schedule. In this manner, we safeguard both heart and sight, reinforcing the fortitude of our citizenry.
Yojana Geete
Behold the drama of a medication that whispers promises of lowered pressure while the eye trembles in silent terror. The nocturnal dip becomes a villain cloaked in darkness, striking when the world is most vulnerable. Only a vigilant guardian can discern the subtle cues and prevent the tragedy.
Jason Peart
Hey folks, just wanted to chime in with a little pep talk about this whole amlodipine‑glaucoma dance. First off, dont panic – most people do fine, the key is keepin an eye on how you feel day to day. If you notice that weird dimming when you stand up, that's a red flag, like a siren blaring in a quiet night. Grab a notebook or your phone and jot down your blood pressure at morning, noon, and bedtime – it’s like keeping a diary for your veins. Share that log with both your GP and eye doc, they’ll be able to tweak the dose or timing, maybe move it to the morning so you dont dip too low overnight. Remember, you’re the captain of your own ship, steering between heart health and vision safety. Stay proactive, stay curious, and above all, stay hopeful – the eyes are resilient when we give them the right support!
Hanna Sundqvist
Honestly, I think pharma pushes amlodipine because they want us glued to watching their ads, not because it’s the safest for glaucoma. They don’t tell you about the midnight blood‑pressure blackouts that can sneak up on you. These big drug companies have their own agenda, and we just end up paying for side‑effects we never signed up for. Do your own research, don’t trust the press release.
Jim Butler
Dear readers, let us embark upon this health journey with vigor and precision. Monitoring your intra‑ocular pressure and systemic blood pressure is the twin pillar upon which ocular preservation rests. Adopt a disciplined schedule for amlodipine dosing, preferably in the early daytime, to avert nocturnal perfusion deficits. Engage your healthcare team proactively; a shared log is the compass that directs optimal therapy. With steadfast commitment, you shall safeguard both heart and sight – onward to clarity! 🌟👁️💪
Ian McKay
The original post contains several instances where commas are missing, leading to run‑on sentences that impede readability. For example, the phrase ‘Amlodipine doesn’t directly raise eye pressure’ should be followed by a semicolon or period before introducing the next clause. Additionally, the list items occasionally lack parallel structure, such as mixing verbs and nouns without consistent tense. Correcting these issues would enhance the professional tone of the article. Consider reviewing the manuscript with a style guide to ensure grammatical consistency.
Deborah Messick
While the attention to punctuation is noted, it distracts from the more pressing ethical oversight evident in the discussion. The article’s failure to emphasize the moral imperative of patient‑centered monitoring borders on negligence. A truly rigorous piece would prioritize safety protocols over typographic perfection. Thus, the focus on commas, though pedantic, should not eclipse the duty to protect vision. Let us, therefore, redirect our scrutiny toward clinical vigilance rather than merely cosmetic edits.