Imagine misplacing your keys every day and then forgetting what the keys are for. Now picture that happening with names, faces, or even the reason you walked into a room. That's daily life for people with Alzheimer's disease or certain types of dementia. The heartbreak isn't just in the forgetting—it's in watching someone’s personality fade over time. Treatments like Exelon offer a glimmer of hope in this relentless struggle. But is Exelon just another pill from a crowded medicine cabinet, or is there something different about how it changes life for those facing memory loss? This story isn’t about magic cures—it’s about the tiny, sometimes overlooked ways a drug can help people hold onto themselves for just a bit longer.
What is Exelon and How Does It Work?
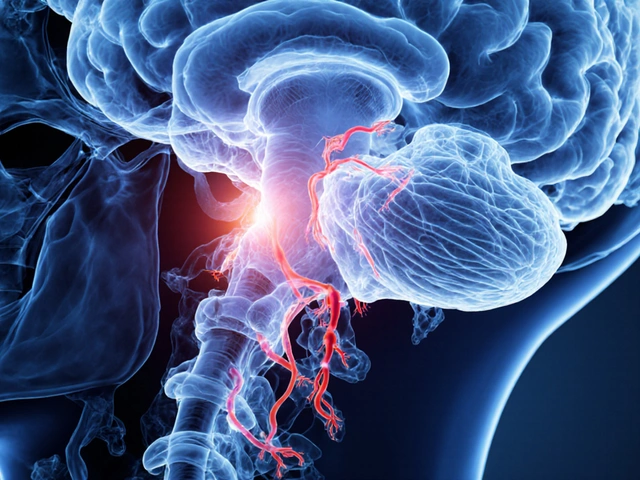
Let’s break down the nuts and bolts first. Exelon, known in the pharmacy as rivastigmine, is part of a group of drugs called cholinesterase inhibitors. These meds don’t turn back the clock on brain damage, but they can slow down the rate at which memory and thinking skills get worse. The basic idea? In brains with Alzheimer’s or Parkinson’s dementia, there’s not enough of a brain chemical called acetylcholine. That’s the stuff that nerves use to talk to each other and keep memories sharp. Exelon works by stopping an enzyme from breaking down this chemical, so there’s more acetylcholine hanging around for brain cells to use.
Why does this matter? Well, studies show that Alzheimer’s patients have up to a 90% drop in acetylcholine. The less they have, the worse their ability to think, remember, and make decisions. With Exelon slowing that breakdown, many patients experience a noticeable difference. They might misplace their wallet less often or have longer moments of clarity. It isn’t a miracle cure, but for family members, seeing a loved one recognize them or tell a simple story matters more than words can describe.
An interesting twist with Exelon: it was the first medication approved as a skin patch for Alzheimer’s (back in 2007). This is a big deal for those who struggle swallowing pills or can’t remember their medicine. The patch releases a steady amount of medication for 24 hours, lowering the spikes and crashes that come with pills. Plus, applying a patch feels a bit less medical and a bit more like self-care, which can make a huge difference in daily life. About 60% of people prescribed Exelon end up using the patch for those reasons.
But there’s more to the story. Exelon is also used for dementia in Parkinson’s disease—one of the few drugs that makes a difference for both Alzheimer’s and Parkinson’s dementia. People with Parkinson’s might move slowly or have a tremor, but as their disease progresses, about half will develop symptoms of dementia. Rivastigmine helps manage the growing confusion, hallucinations, and memory slips. It’s not a full stop, but for many families, it can mean the difference between continuing to live safely at home versus needing extra care.
The science isn’t all sunshine and rainbows—most people only see mild improvements, and the drug doesn’t work for everyone. Clinical studies found that about half of patients will see some benefit, particularly in memory and basic daily function, over 6 to 12 months. After that, the disease continues its course, but starting Exelon early gives people more quality time before decline picks up speed. It’s also not a one-size-fits-all solution. Some people are more sensitive to side effects, and the drug has to be slowly increased (titrated) to prevent stomach upset.
Beyond science, Exelon’s impact shows up in the smallest daily victories—like remembering to feed the cat in the morning or having a calm dinner conversation. I've seen families here in Melbourne organize reminder boards, set timer alarms, and use pet feeding schedules with their loved one’s patch routine. Pallas, my Persian cat, is a pro at letting me know when it’s time for meals—which might be why I always remember to change her litter box (and sometimes wish caring for a human brain was half as simple).

Benefits and Limitations of Exelon Treatment
Now to the real-life part—how does Exelon actually help, and where does it fall short? The clearest effect, according to both doctors and family members, is on memory. Some people notice that daily tasks become simpler—getting dressed, making a cup of tea, following along with a conversation. It’s the moments when someone remembers a child’s birthday, a favorite song lyric, or a joke from decades ago. Exelon doesn’t bring back the past, but it often helps keep the present from slipping away quite so fast.
One standout benefit comes from research done in 2021 at the University of Melbourne. They ran a community study where older people with mild-to-moderate Alzheimer’s joined social programs alongside starting Exelon. The group that combined medicine plus social support performed better than those who just took pills at home. That suggests Exelon’s best trick isn’t just in chemical tweaks, but also in buying time for brain-engaging routines that keep people connected to their world.
But you can’t ignore the challenges. Exelon, especially as a pill, is known for causing some nasty stomach issues—nausea, vomiting, and even weight loss. That’s why a lot of doctors recommend starting with the lowest possible dose and slowly building up. For folks who already have trouble with eating or keeping weight on, these side effects can overshadow the drug’s benefits. That’s another reason the patch version is so popular: because it gently releases the medication over time, those gut symptoms are much less intense.
Some patients on Exelon notice more than just memory changes. The drug can also help with so-called “activities of daily living.” That means practical stuff—managing hygiene, preparing meals, or handling money. In severe cases, it can delay when someone needs to move into full-time care. There’s even a bit of evidence that Exelon reduces nighttime confusion or wandering, which are especially tough for caregivers to handle alone.
But let’s be honest, Exelon isn’t a shield against all of dementia’s attacks. The disease still progresses, and for about half of users, the improvements are minimal or even hard to spot. Sometimes families notice their loved one is calmer or less agitated—but others might experience extra confusion or anxiety, especially in the beginning. Tracking these changes, keeping a daily log, and regularly chatting with the doctor can make all the difference in fine-tuning treatment.
Patients and families sometimes ask if Exelon changes someone’s personality or just masks symptoms. From what I’ve seen, it’s less about changing who someone is, and more about turning up the volume on their best self for a little longer. One Melbourne family described it this way: "When Mum started the patch, she started singing again in the kitchen. It wasn’t about memory. She just had more of her spark back."
Insurance and cost are another real challenge. The Exelon patch is more expensive than generic pills, and some people face tough out-of-pocket costs, even with coverage. But doctors will often help families navigate this—by using prescription assistance programs or by switching between the patch and pills at different times.
If you’re just starting Exelon or caring for someone who is, here are some tips from real families and dementia support groups in Australia:
- Always apply the patch to clean, dry, hairless skin—rotate sites (like upper back, chest, or upper arm) to avoid irritation.
- If using pills, try dosing with meals to minimize nausea. If you miss a dose by several hours, wait until the next scheduled dose—don’t double up.
- Keep a medication journal to track effects, side effects, and daily routines. Share this with your doctor to adjust as needed.
- Combine medication with brain-active routines: walking, music, games, social meetups—even pet care can help boost mood and connection.
- If someone struggles with patches peeling off, use a medical adhesive (pharmacies sell gentle patches meant just for that).
- Set visual reminders in prominent spots—digital clocks, smart assistants, or sticky notes by the refrigerator. Pallas likes to nap on our reminder board, so I never forget her treats—or an Exelon patch change.
Some families report increased anxiety, agitation, or rare allergic reactions. If this happens, call your doctor right away. If you notice heart rate irregularities (Exelon can slow down the heart a bit), headaches, bad dreams, or sudden changes in energy, don’t just wait it out—better safe than sorry.

Living with Exelon: Real-World Advice and Support
When you’re living with dementia—or caring for someone who is—life quickly becomes more about routines than rigid plans. Small adjustments matter. So how does Exelon fit into all this, day after day? Here’s the real scoop from what I’ve seen, heard, and lived in Melbourne and beyond.
Because Exelon takes several weeks to kick in, patience is key. Doctors usually start low and go slow with the dosage. That gives the brain a chance to adjust and helps spot any side effects early. Most families notice changes after four to six weeks, not overnight. The improvements tend to be subtle—cleaner conversations, a little less repetition, sometimes better focus. Celebrate these moments. It’s easy to focus on what’s lost, but even a few stolen moments of clarity can become lifelines in the daily grind.
The patch has turned out to be a secret weapon for lots of folks. Forgetful patients who miss labelling bottles or mixing up pillboxes find it’s a lot harder to overlook a patch stuck right onto their skin. Some adult children put stickers by the bathroom mirror or set alarms on mobile phones—one family even recorded their dog barking to remind Mum it was Patch Time (and no, sadly, Pallas doesn’t help with tech). When routines become rituals, like putting on socks or brushing teeth, it’s easier for patients to manage their own care, even as memory slips away.
Caregivers face their own set of headaches. Managing Exelon means paying attention to water intake (to fight dehydration from stomach side effects), watching for skin reactions, and juggling doctor’s appointments. Support groups swap advice: some use hypoallergenic creams if the patch site gets itchy; others schedule patch changes right after a shower when the skin is cleanest. In the summer, when sweat and sunshine can loosen adhesive, trying different body areas or extra stick-on medical tape helps.
Diet and hydration can make a surprisingly big difference. Because Exelon can upset the stomach, eating frequent small meals and drinking extra water works for most people. Avoiding spicy or rich foods when starting out can help. It’s also smart to weigh yourself (or your loved one) once a week. If you notice rapid weight loss, call your doctor—sometimes adjusting dosage, route, or medication timing stops this before it becomes a bigger issue.
One thing that rarely gets discussed enough is mental health. It’s easy for people with dementia—and those caring for them—to feel isolated or overwhelmed, especially when progress slows or setbacks pop up. In Melbourne, local dementia cafés, senior clubs, and online forums give families a way to vent, swap tips, and laugh about little triumphs (like finding the TV remote before anyone panics). Connecting in person, by phone, or even through digital communities has a bigger impact than any medicine alone.
Doctors here recommend regular check-ins—at least every 3 to 6 months—to re-evaluate if Exelon is still helping. Sometimes, as the disease progresses, other medicines or therapies might be needed. But sticking with the routine, staying flexible, and celebrating small wins makes a real difference.
There are a few special cases to keep in mind. If you or your loved one has a history of heart disease, stomach ulcers, seizures, or asthma, tell your doctor before starting Exelon. The drug can interact with these conditions in unexpected ways. Also, unrelated meds—like beta-blockers, anticholinergics, and other memory drugs—might throw a wrench into the works, so keep an updated meds list handy.
The most important thing? Exelon isn’t about chasing lost time. It’s about making today better—even if that just means finishing a crossword, remembering a grandchild’s laugh, or sharing a quiet moment with a pet. With the right support and adaptation, people on Exelon can often do more for themselves, and families can hold onto ordinary joy a bit longer.




Jason Layne
It is astonishing how the pharmaceutical conglomerates push Exelon as a miracle while hiding the cascade of side‑effects that only they can truly quantify. The patch, they claim, is a convenience, yet it embeds a slow‑release system that could be used to monitor patient compliance for future data harvesting. Their marketing teams, funded by clandestine offshore accounts, purposefully downplay the gastrointestinal distress that the oral form can provoke, steering the vulnerable toward a more lucrative patch market. Moreover, the alleged “dual‑action” on Parkinson’s dementia is a thin veneer to broaden the drug’s patent life, extending corporate profit cycles by another decade. Clinical trials, often ghost‑written, selectively publish the modest cognitive gains while omitting the dropout rates caused by nausea, vomiting, and weight loss. It is no coincidence that the patent for rivastigmine was renewed shortly after the patch’s introduction, coinciding with a surge in insurance reimbursements that strain public health budgets. The patch’s adhesive, marketed as hypoallergenic, contains polymeric compounds that can cause sub‑clinical dermatitis, a fact suppressed in patient brochures. While doctors are told to “start low and go slow,” the incremental titration schedule is designed to keep patients in a perpetual state of dependence on dose adjustments, ensuring continuous pharmacy visits. Some neurologists, incentivized by speaker fees, tout anecdotal improvements that are statistically indistinguishable from placebo effects. The reality is that half of the patients experience negligible benefit, yet the narrative of hope is perpetuated to sustain market demand. The hidden cost is not just financial; it is the psychological burden imposed on families who cling to false expectations. The drug’s interaction profile with anticholinergic agents is deliberately obfuscated, leading to dangerous polypharmacy scenarios that further entrench patients in the healthcare system. In essence, Exelon’s presence on the market reflects a calculated strategy to monetize incremental symptom management rather than genuine disease modification. The patch’s “steady release” is a euphemism for a steady stream of revenue to the pharmaceutical elite, who will stop at nothing to preserve their bottom line. Critics who raise these points are often dismissed as “conspiracy theorists,” yet the patterns of secrecy and profit‑first motives are evident to any diligent observer.
Hannah Seo
For anyone beginning Exelon, it helps to keep a simple medication log. Write down the time you change the patch and note any stomach upset or skin irritation. Share this log with your doctor during each visit; it guides dose adjustments and can catch side effects early. Pair the medication with daily routine activities like short walks, music, or puzzles – the brain benefits from consistent engagement. Most families find that setting a reminder on a phone or a sticky note on the fridge reduces missed doses and eases caregiver stress.
Victoria Unikel
i guess the patch just kinda works sometimes.
Lindsey Crowe
Sure, because a tiny patch is the answer to all the complexities of dementia. It’s almost comical how we celebrate a marginal improvement as if it were a breakthrough. Meanwhile, the real issues – caregiver burnout, cost, and limited efficacy – get swept under the rug. If only we could patch those problems away too.
Rama Hoetzlein
Let us contemplate the paradox: a drug that claims to ‘slow’ a relentless decay while the very industry accelerates its own dominion. Exelon, in its patch‑form, becomes a symbol of the commodification of human cognition – a glossy adhesive that binds not just to skin, but to profit margins. 🌐 The aggressive marketing of ‘dual‑action’ for Parkinson’s dementia masks an underlying agenda to extend patent lifespans and lock patients into perpetual consumption. One must question whether the subtle benefits observed are genuine or merely a curated placebo, meticulously crafted by a network of funded researchers. The ethical breach lies not in the chemistry but in the narrative spun to comfort desperate families, diverting them from systemic reform.