Potassium Risk Calculator
Calculate Your Potassium Risk
Based on your kidney function and potassium levels, this tool assesses your risk when using potassium-based salt substitutes with blood pressure medications.
Most people think switching to a salt substitute is a smart move for their heart. It’s marketed as healthier, lower in sodium, and even promoted by doctors for high blood pressure. But if you’re taking an ACE inhibitor or an ARB, that tiny shaker on your table could be quietly putting your life at risk.
What’s Really in Those Salt Substitutes?
Regular table salt is sodium chloride. Salt substitutes swap out some or all of that sodium for potassium chloride. Products like LoSalt or NoSalt Lite aren’t just "less salty"-they’re loaded with potassium. Some contain up to 66% potassium chloride. That means every teaspoon you use adds nearly 600 mg of potassium to your diet. For someone eating normally, that’s a big jump.
Most people don’t realize how much potassium they’re getting. The average adult needs about 2,600-3,400 mg per day. A single teaspoon of potassium-based salt substitute can push you 20% closer to your daily limit. Add that to bananas, potatoes, spinach, and beans-and you’re flirting with danger if your kidneys can’t keep up.
Why ACE Inhibitors and ARBs Are the Problem
ACE inhibitors (like lisinopril, enalapril) and ARBs (like losartan, valsartan) are among the most common blood pressure medications. They work by relaxing blood vessels and reducing fluid buildup. But here’s the catch: they also reduce a hormone called aldosterone. Aldosterone tells your kidneys to flush out potassium. When it drops, potassium builds up.
That’s fine if your kidneys are working well. But if they’re not-because of diabetes, aging, or chronic kidney disease-your body can’t get rid of the extra potassium fast enough. And when you add a potassium-rich salt substitute on top? That’s when levels spike.
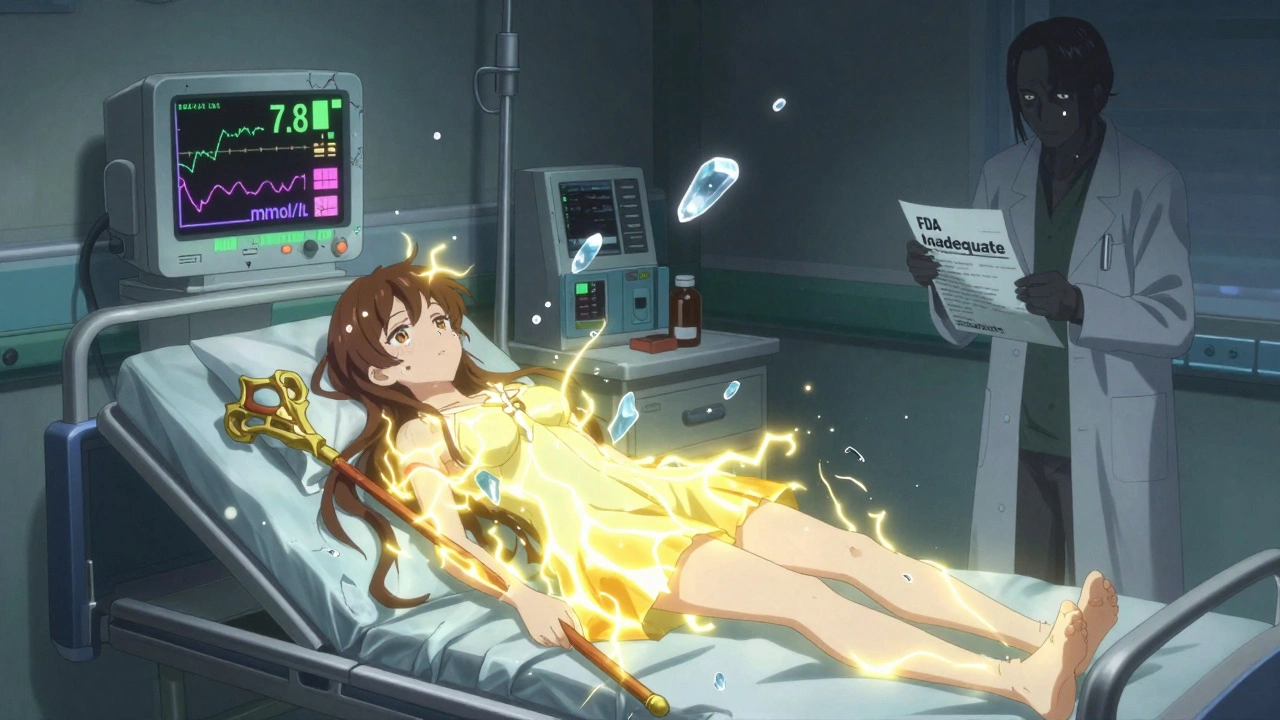
Hyperkalemia-high potassium in the blood-is silent until it’s too late. You might feel nothing. Or you might get muscle weakness, irregular heartbeat, or sudden cardiac arrest. A 2004 case report in the Journal of the Royal Society of Medicine documented a 72-year-old man who went into cardiac arrest after using LoSalt while on lisinopril. His potassium level hit 7.8 mmol/L. Normal is 3.5-5.0. Above 6.5? That’s life-threatening.
Who’s Most at Risk?
You’re not equally at risk. It depends on your kidneys.
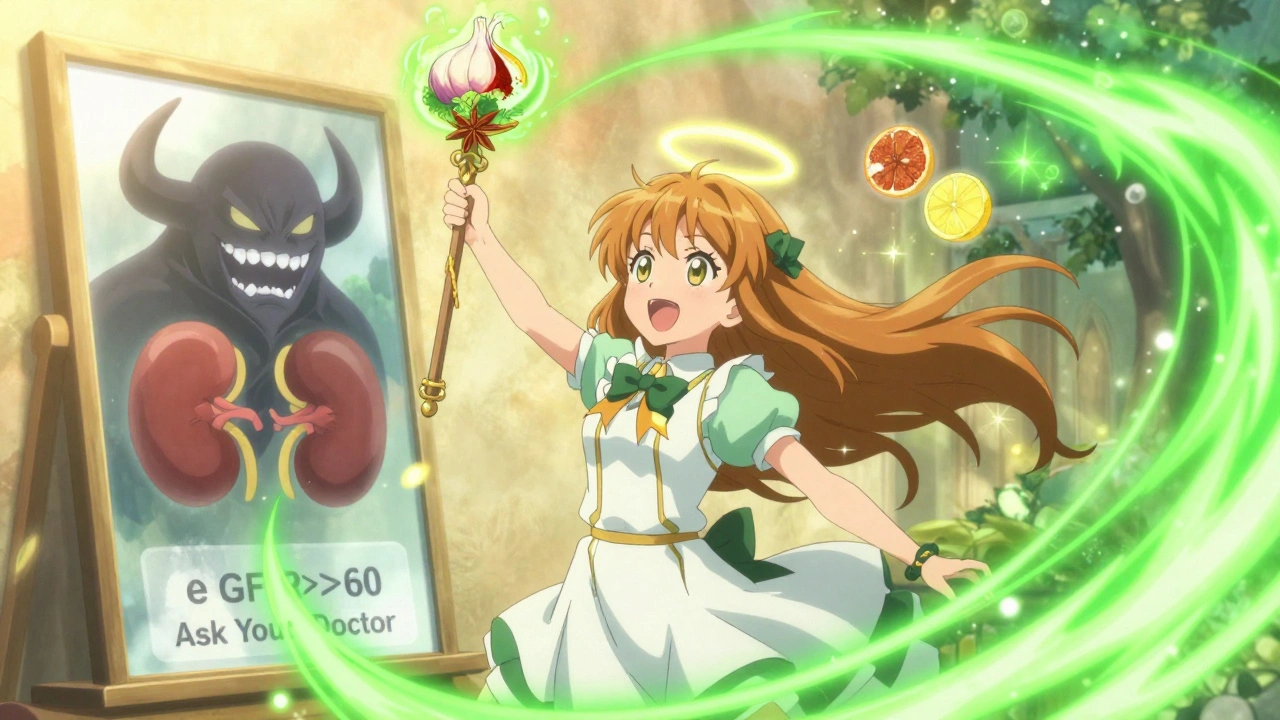
- If your eGFR (kidney function) is above 60 mL/min/1.73m², you’re likely fine. Studies show potassium substitutes can even lower stroke risk in healthy people.
- If your eGFR is below 60-about 1 in 7 adults-you’re in danger. That’s chronic kidney disease stage 3 or worse.
- Diabetics? Even higher risk. Up to 20% have a condition called hyporeninemic hypoaldosteronism, which makes them extremely sensitive to potassium buildup.
And here’s the scary part: 78% of people on ACE inhibitors or ARBs don’t even know they need to avoid potassium salt substitutes. A 2023 study in JAMA Internal Medicine found most patients weren’t warned. Not by their doctor. Not by the label. Not even by the pharmacist.
Real Stories, Real Consequences
Reddit threads are full of them. One user, with 4,200 karma in the r/kidney_stones community, wrote: "Woke up in the ER with potassium at 6.3 after using Heart Salt for three weeks while on lisinopril." Another user on Drugs.com, age 68, said: "Severe muscle weakness and irregular heartbeat. My doctor said I nearly died."
On Amazon, 7% of reviews from people who self-identify as having kidney problems say their doctor told them to stop the salt substitute after blood tests showed high potassium. These aren’t outliers. They’re symptoms of a system failure.
What About the Benefits? Aren’t Salt Substitutes Good for You?
Yes-for most people. A landmark 2025 JAMA study followed 21,000 people for five years. Those using a salt substitute with 25% potassium chloride had a 14% lower risk of stroke. That’s huge. And it’s why the American Heart Association is updating its guidelines to recommend them for people with normal kidney function.
But here’s the split: 85-90% of the population can use them safely. The other 10-15%? They’re the ones getting hurt. And they’re the ones nobody tells.
What Should You Do?
If you’re on an ACE inhibitor or ARB, here’s your action plan:
- Check your eGFR. Ask your doctor for your latest kidney function number. If it’s below 60, avoid potassium salt substitutes.
- Check your potassium level. If it’s above 4.5 mmol/L, stop using them immediately.
- Read the label. Look for "potassium chloride" on the ingredients. If it’s there, don’t use it unless your doctor says it’s safe.
- Ask your doctor: "Is it safe for me to use salt substitutes?" Don’t assume they know you’re using one.
And if you’re trying to cut sodium? There are safer ways. Use herbs and spices. Try Mrs. Dash, garlic powder, smoked paprika, lemon zest, or black pepper. You can reduce sodium by 40-50% without touching potassium at all.
Why Isn’t This Better Warned?
Only 3 out of 12 major salt substitute brands in the U.S. warn about interactions with ACE inhibitors or ARBs. The FDA doesn’t require it. Canada did-starting January 2024. The U.S. is lagging.
In September 2023, an FDA official testified that current labeling is "inadequate for high-risk populations." A proposed rule to fix this is expected in mid-2026. Until then? You’re on your own.
And cost? Potassium salt substitutes cost 2-3 times more than regular salt. You’re paying more for a product that could kill you if you’re not careful.
The Bottom Line
Salt substitutes aren’t universally good or bad. They’re tools. And like any tool, they can help-or hurt-depending on how you use them.
If you have healthy kidneys and no kidney disease, they’re a smart choice. If you’re on blood pressure meds like lisinopril, losartan, or similar? They’re a hidden threat.
Don’t trust the marketing. Don’t assume your doctor knows. Don’t wait for symptoms. Ask for your eGFR and potassium levels. Check your salt substitute label. And if you’re unsure? Stick with herbs, spices, and plain old table salt-used sparingly.
Your heart might thank you. But your kidneys? They’re the ones keeping you alive.




Paul Dixon
Man, I had no idea this was a thing. I’ve been using NoSalt for years since my BP went up. Guess I’m lucky my kidneys are still good, but I’m getting my eGFR checked tomorrow. Thanks for laying this out so clearly.
Courtney Blake
Of course the FDA won’t do anything until someone dies. Corporations make billions off these ‘health’ products and no one wants to scare people away from buying them. This is capitalism in action: profit over people.
matthew dendle
so u mean like… potassium is bad? wow. who knew. next u’ll tell me water can kill u if u drink too much. 🙄
Monica Evan
I’m a renal dietitian and I see this all the time. Patients think ‘natural’ = safe. Salt substitutes are labeled ‘heart-healthy’ but the fine print? Gone. I hand out little cards to my patients with the top 5 hidden potassium traps. You’re not alone if you didn’t know this.
Also-Mrs. Dash is your BFF. So is cumin. And lime juice. No magic pills, just real flavor.
Lisa Stringfellow
Why do people keep ignoring the science? You’re telling me 78% of people on these meds are just… unaware? And nobody’s doing anything? This is a waiting room for cardiac arrest.
Mia Kingsley
Oh so now we’re blaming salt substitutes? What’s next? Is coffee gonna give you kidneys? You know what’s really dangerous? Trusting big pharma to tell you what’s safe.
Kristi Pope
This is such an important post. I shared it with my mom who’s on losartan. She’d been using LoSalt for years. We’re both going to the doctor next week to check her potassium. Thank you for being the voice no one else is.
john damon
⚠️ I just checked my spice rack. LoSalt. 😳 I’m so glad I read this. Thanks for the heads up. My heart is beating normally right now… I think.
Jimmy Kärnfeldt
It’s funny how we’re taught to fear sodium but never taught to question potassium. We’re so conditioned to think ‘less salt = better’ that we don’t stop to ask what’s replacing it. This is a wake-up call for the whole system.
Ariel Nichole
My dad had a scare last year with high potassium. They didn’t tell him about the salt substitute. He’s been using herbs since. He says his food tastes better now anyway.
Eddie Bennett
I’m 62, on lisinopril, and my eGFR is 58. I’ve been using LoSalt for 3 years. I’m getting my potassium checked today. This could’ve been a death sentence I didn’t know I was holding.
Vivian Amadi
Stop using salt substitutes. That’s it. No debate. You’re not special. Your kidneys aren’t magic. Just use pepper.
Sylvia Frenzel
It’s not just salt substitutes. It’s the entire medical system. Doctors don’t have time. Pharmacists don’t read labels. Patients don’t ask. And the FDA? They’re asleep at the wheel. This isn’t an individual failure-it’s institutional.
Aidan Stacey
I’ve been telling people this for years. One guy told me he’d rather die than give up his ‘healthy’ salt. I didn’t argue. I just handed him a jar of smoked paprika and walked away. Some people need to learn the hard way.