Cyclosporine: Uses, Risks, and What You Need to Know
When you hear cyclosporine, a potent immunosuppressant drug used to prevent organ rejection and treat autoimmune disorders. Also known as Neoral or Sandimmune, it works by quieting down your immune system so it doesn’t attack your new kidney, liver, or heart. But this drug isn’t a simple fix—it’s a balancing act. Take too little, and your body might reject the transplant. Take too much, and you risk kidney damage, high blood pressure, or even cancer.
Cyclosporine doesn’t work alone. It often sits in the middle of a drug cocktail. For example, it’s commonly paired with azathioprine, another immunosuppressant that reduces the chance of rejection, or with steroids like prednisone. But mixing it with other meds can be dangerous. Like amiodarone, a heart rhythm drug that can spike cyclosporine levels to toxic amounts, or even common antibiotics like erythromycin. These aren’t theoretical risks—they’ve sent people to the ER. That’s why blood tests to check cyclosporine levels aren’t optional. They’re life-saving.
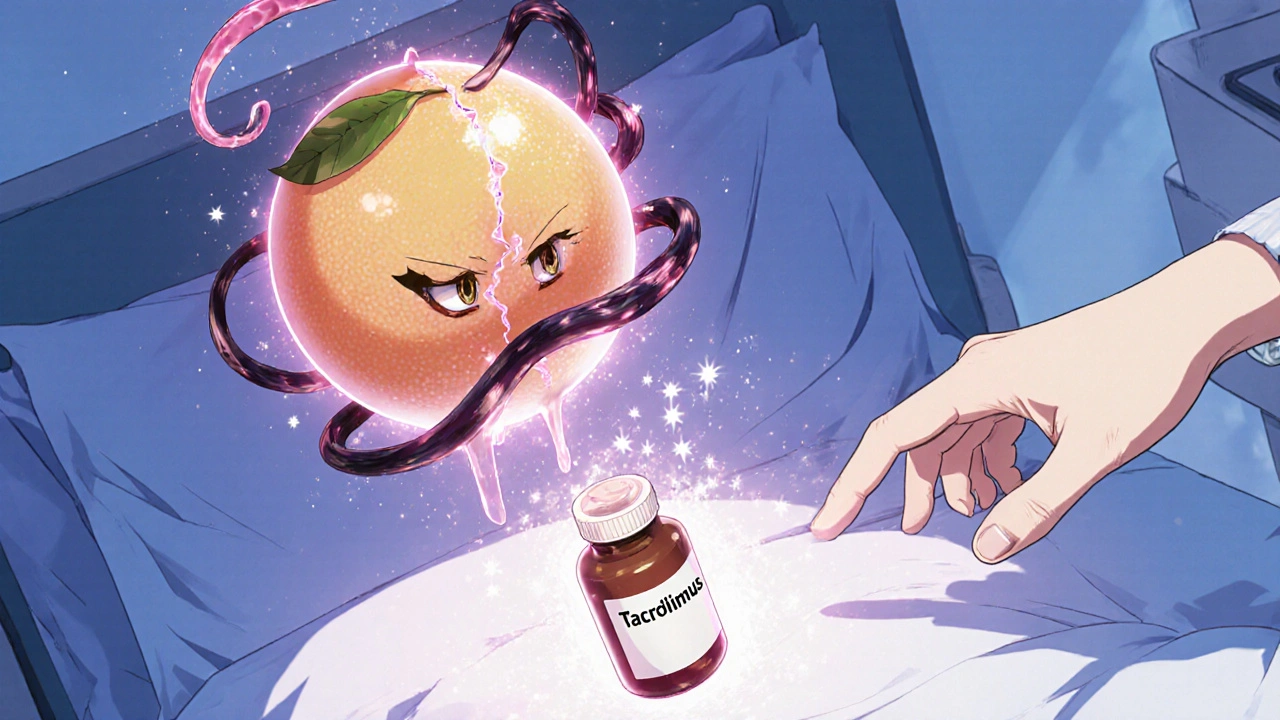
It’s not just about transplant patients. Cyclosporine is also used for severe psoriasis, rheumatoid arthritis, and even some cases of eczema when other treatments fail. But it’s not for everyone. If you have kidney disease, high blood pressure that won’t budge, or a history of skin cancer, your doctor will think twice. And if you’re drinking grapefruit juice? Stop. It interferes with how your body breaks down the drug, turning a safe dose into a dangerous one.
What you’ll find in this collection isn’t just a list of articles. It’s a practical toolkit. You’ll see how cyclosporine fits into the bigger picture of immune suppression—how it compares to newer drugs, why monitoring matters more than dosage alone, and how it connects to other conditions like blood clots or liver stress. No fluff. No theory without application. Just what you need to understand the drug, spot the red flags, and talk smarter with your care team.