Immunosuppressants: What They Are, How They Work, and What You Need to Know
When your immune system turns against your own body—attacking healthy tissue, rejecting a transplanted organ, or overreacting to harmless substances—you might need immunosuppressants, medications that reduce the activity of the immune system to prevent damage. Also known as anti-rejection drugs, they’re not meant to cure disease, but to keep your body from fighting itself too hard. These drugs are critical for people who’ve had kidney, liver, or heart transplants. Without them, the body sees the new organ as an invader and tries to destroy it. But they’re also used for conditions like lupus, rheumatoid arthritis, and Crohn’s disease, where the immune system mistakenly attacks joints, skin, or the gut.
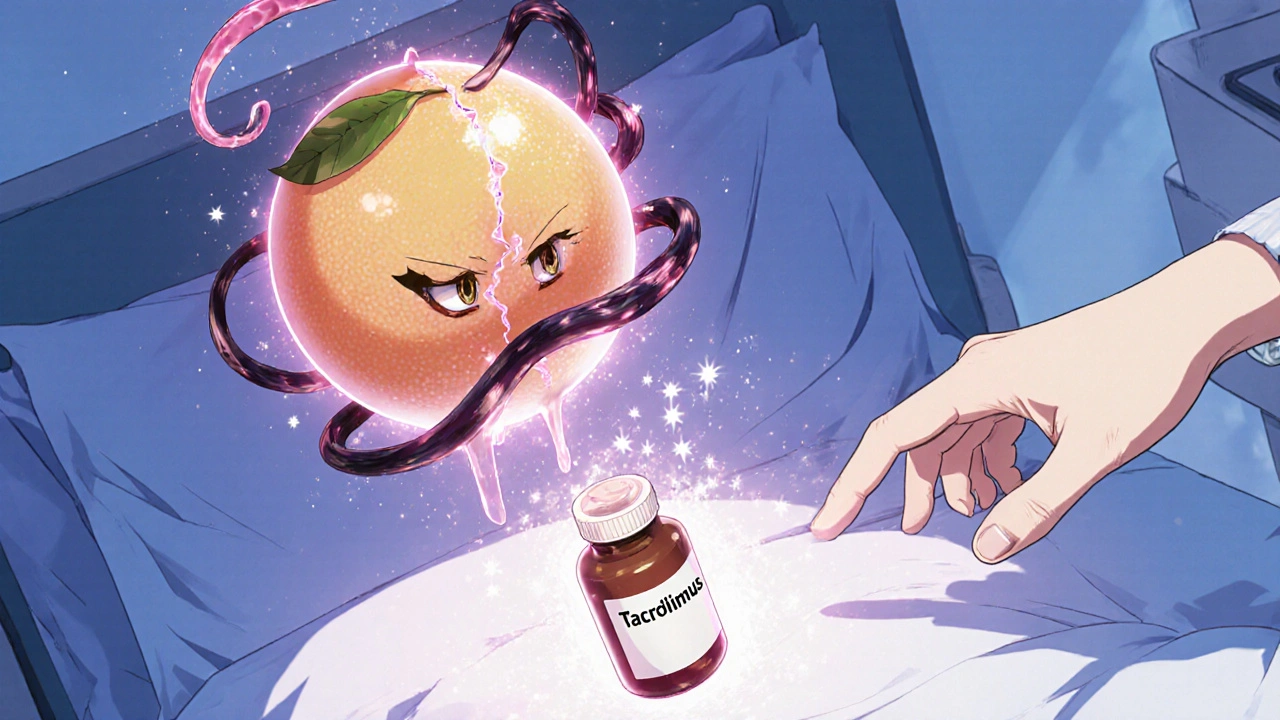
There are several main types of immunosuppressants, drugs that lower immune system activity to prevent tissue damage. Corticosteroids, like prednisone, are often the first line of defense—they reduce inflammation fast but come with weight gain, bone loss, and blood sugar spikes over time. Then there’s azathioprine, a long-term immunosuppressant used to maintain control after initial treatment. It’s older but still widely used, especially in transplant patients, though it can lower white blood cell counts and raise clot risk. Other common ones include cyclosporine, tacrolimus, and mycophenolate, each with different side effects and monitoring needs.
These drugs don’t work the same for everyone. Your doctor will pick one based on your condition, other meds you take, and your risk for infections or cancer. That’s why you’ll need regular blood tests—sometimes every few weeks—to check liver function, kidney health, and blood cell levels. You can’t just stop taking them, even if you feel fine. Suddenly stopping can trigger a dangerous flare-up of your disease or organ rejection. And because your immune system is turned down, even a cold or flu can become serious fast. That’s why vaccines, handwashing, and avoiding sick people aren’t optional—they’re part of your treatment plan.
Some of the posts here dive into how azathioprine might raise the risk of blood clots, why steroid slurry treatments work for certain immune-driven conditions, and how drugs like budesonide are used differently than older steroids. Others explain how immune responses interact with gene therapy or why medical alert bracelets matter when you’re on long-term immunosuppressants. You’ll find real-world guidance on managing side effects, spotting warning signs, and making sense of the trade-offs. This isn’t theory—it’s what people actually deal with when their immune system needs to be held in check.