Understanding Tendonitis: An Introduction
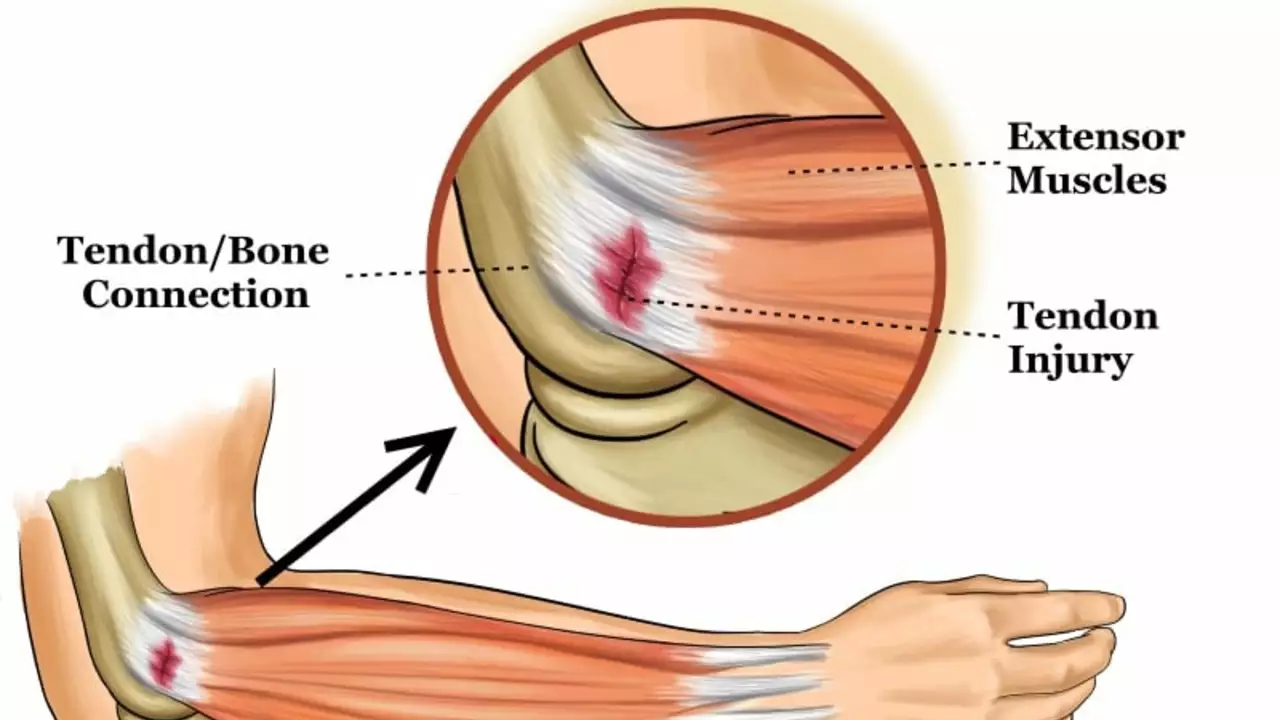
As a swimmer, your body goes through a lot of physical stress, especially in your shoulders, elbows, knees, and ankles. One common injury that you may encounter is tendonitis. Tendonitis is an inflammation or irritation of a tendon, the thick fibrous cords that attach muscle to bone. The condition can cause pain and tenderness just outside a joint. Before we delve into the specifics of tendonitis in swimmers, let's first understand what tendonitis is and how it affects your body.
The Causes of Tendonitis in Swimmers
Tendonitis in swimmers is often caused by overuse of the tendons during intensive training sessions. When you swim, your body uses a lot of repetitive motions. This can put a lot of strain on your tendons, especially if you're not giving them enough time to recover. Other factors that could contribute to the development of tendonitis include poor technique, insufficient warm-up before training, and inadequate equipment, such as swimwear that is too tight or goggles that don't fit properly.
Recognizing the Symptoms of Tendonitis
One of the primary symptoms of tendonitis is a gradual buildup of pain around the affected area. This pain often worsens when you move the affected limb or joint. Other symptoms that you might experience include tenderness, mild swelling, and a sensation of grating or crackling when you move the affected area. If you notice any of these symptoms, it's important to take a break from swimming and rest. If the symptoms persist, it's important to seek medical attention.
Diagnosing Tendonitis in Swimmers
When you visit a doctor, they'll likely start by asking you about your symptoms and medical history. They'll then carry out a physical examination to check for any signs of tendonitis. This might involve moving your joint in different directions to see if it's causing you any discomfort. In some cases, your doctor might also recommend imaging tests, such as an X-ray or ultrasound, to get a better look at your tendon.
Treatment Options for Tendonitis
The treatment for tendonitis generally involves relieving pain and reducing inflammation. This might involve taking over-the-counter pain relievers, applying ice to the affected area, and avoiding activities that can worsen your symptoms. Your doctor might also recommend physical therapy to strengthen your muscles and improve your flexibility. In severe cases, surgery might be necessary to repair the damaged tendon.
Preventing Tendonitis in Swimmers
Prevention is always better than cure, and this is especially true when it comes to tendonitis. To prevent tendonitis, it's important to warm up properly before you start swimming. This can help to prepare your muscles and tendons for the physical activity ahead. It's also important to use correct technique when you're swimming. This can help to distribute the physical strain evenly across your body, reducing the risk of overuse injuries.
Swimming with Tendonitis: What You Need to Know
If you have tendonitis, it's important to take it easy and not to push yourself too hard. Overworking an inflamed tendon can lead to further injury and prolong your recovery. While it might be frustrating to take a step back from your training, remember that resting is an important part of healing. Once your symptoms have improved, you can gradually start to increase your activity levels again, but be sure to do this slowly to avoid aggravating your tendonitis.
Conclusion: Taking Care of Your Body as a Swimmer
As a swimmer, your body is your most important tool. It's crucial to take good care of it and to listen to it when it's telling you something is wrong. Remember, a temporary setback like tendonitis is just that - temporary. With the right treatment, and by taking the appropriate precautions, you'll be back in the pool before you know it.



Jessica Taranto
Great rundown, thanks for the clarity.
akash chaudhary
The article correctly identifies overuse as the primary catalyst for tendonitis, but it neglects to emphasize the biomechanical imbalances that often precipitate the condition. Swimmers frequently exhibit excessive internal rotation of the shoulder, which increases shear forces on the rotator cuff tendons. Moreover, inadequate scapular stabilization contributes to maladaptive loading patterns. The omission of periodization strategies is another glaring oversight; progressive overload must be meticulously planned to allow tissue adaptation. A proper warm‑up should incorporate dynamic shoulder articulation, not merely static stretches. Ice application post‑training offers symptomatic relief, yet it does not address the inflammatory cascade at a cellular level. NSAIDs provide analgesia, but reliance on pharmacologic intervention can mask underlying technique flaws. Physical therapy protocols must integrate eccentric strengthening, which has been shown to remodel tendon collagen orientation. Additionally, the role of nutrition-particularly omega‑3 fatty acids-in modulating inflammation warrants discussion. Swimmers should also examine equipment ergonomics; a poorly fitted hand paddle can exacerbate tendon loading. The recommendation for imaging is sound, but ultrasound offers real‑time assessment of tendon gliding, surpassing static X‑ray in utility. Lastly, the piece fails to mention the psychological impact of forced rest periods on athlete motivation, an aspect that coaches must manage. In sum, while the guide offers a solid foundation, it requires a more nuanced exploration of preventive biomechanics, therapeutic modalities, and athlete management strategies.
Adele Joablife
I appreciate the emphasis on proper warm‑ups; many swimmers skip that step thinking it’s optional. Adding a few minutes of arm circles and band pull‑aparts can dramatically reduce tendon strain. Also, integrating cross‑training like yoga helps maintain flexibility without overloading the same joints. Just remember to listen to your body and back off if you feel a twinge. Consistency in technique is key to long‑term health.
kenneth strachan
Whoa, this sounds like a drama‑free zone, but we all know the pool can be a battlefield! If you ignore that nagging pain, you’ll end up crying on the deck.
Mandy Mehalko
Stay positive, swimmers! Tendonitis is just a bump in the road, and with the right rehab you’ll bounce back stronger than ever. Keep your head up and trust the process.
Bryan Kopp
Sounds like a solid plan. Rest, ice, and gradual load‑increase are the basics.
Patrick Vande Ven
From a clinical standpoint, the recommendation to seek imaging only after persistent symptoms aligns with evidence‑based practice. Ultrasound, in particular, provides dynamic insight into tendon behavior during motion, which is invaluable for differential diagnosis.
Tim Giles
Furthermore, the diagnostic algorithm should incorporate patient‑reported outcome measures such as the VISA‑A score to quantify functional impairment. This facilitates objective monitoring throughout the rehabilitation timeline and ensures that therapeutic adjustments are data‑driven rather than anecdotal.
Peter Jones
I’d add that low‑impact cardio, like stationary biking, maintains aerobic fitness while giving the inflamed tendon a breather. It’s a win‑win for overall conditioning.
Gerard Parker
Great points all around. In addition to ice, consider contrast therapy-alternating hot and cold packs-to boost circulation. Also, a certified swim coach can fine‑tune your stroke mechanics, which often reduces undue stress on the shoulder girdle.
Thomas Burke
Don’t forget to hydrate! Proper fluid balance aids tissue recovery and helps keep inflammation in check.
Debbie Frapp
Quick grammar check: "adequate" not "adeqaute"-just a tiny typo in the equipment section.
Michelle Abbott
Whilst the discourse delineates prophylactic maneuvers, the omission of proprioceptive neuromuscular facilitation (PNF) protocols is conspicuous.
Heather Jackson
Oooo, love the fancy terminology! But seriously, adding PNF stretches could be a game‑changer for those stiff shoulders.
Akshay Pure
One might argue that the article caters to the average swimmer, yet elite athletes demand a more granular approach, replete with periodization schemata and load‑monitoring analytics.
Steven Macy
It’s fascinating how our bodies signal distress; tendon pain is a reminder of the delicate balance between ambition and capability.
Matt Stone
Rest is key.
Joy Luca
While brevity is appreciated, oversimplifying the rehab protocol can mislead novices; a structured, progressive loading plan is essential.
Jessica Martins
The content is well‑structured and informative.
Doug Farley
Oh wow, “well‑structured,” you say-because we haven’t seen that claim a million times before. 🙄