Introduction to Functional Dyspepsia and Spicy Foods
As a lover of spicy foods, I've always been curious about the effects they have on our digestive system. In particular, I wanted to explore the connection between spicy foods and functional dyspepsia, a common gastrointestinal disorder characterized by symptoms such as bloating, discomfort, and indigestion. In this article, I'll share the findings of my research and discuss the impact that spicy foods can have on functional dyspepsia.
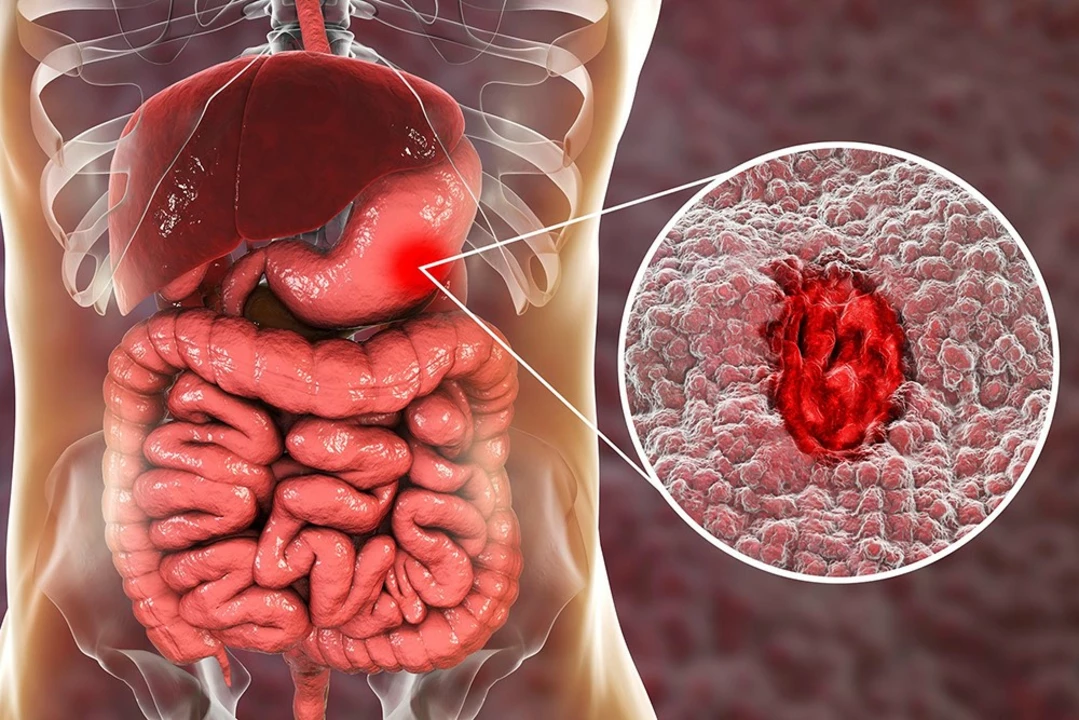
Understanding Functional Dyspepsia
Functional dyspepsia, also known as non-ulcer dyspepsia or indigestion, is a common gastrointestinal disorder that affects around 20% of the population. It is characterized by symptoms such as epigastric pain or discomfort, bloating, early satiety, and an overall feeling of fullness. The exact cause of functional dyspepsia is still unknown, but researchers believe that it may be related to an abnormal response to gastric distention, altered gastrointestinal motility, or heightened visceral sensitivity.
Can Spicy Foods Trigger Functional Dyspepsia?
There's no denying that spicy foods can cause a certain level of discomfort for some people, especially those with sensitive stomachs. But can they actually trigger functional dyspepsia? Studies suggest that the consumption of spicy foods may exacerbate symptoms of functional dyspepsia, but it's unclear whether they can directly cause the condition. It's important to note that the effects of spicy foods can vary greatly from person to person, so while some individuals may experience worsening symptoms after consuming spicy foods, others may not be affected at all.
Why Spicy Foods May Cause Discomfort
Spicy foods get their heat from a compound called capsaicin, which is found in chili peppers. When consumed, capsaicin can irritate the lining of the stomach and intestines, causing a burning sensation and increasing the production of gastric acid. This can lead to symptoms such as heartburn, indigestion, and abdominal pain – all of which are associated with functional dyspepsia. Additionally, spicy foods may also slow down the emptying of the stomach, which can contribute to feelings of fullness and bloating.
Managing Functional Dyspepsia Symptoms
If you're suffering from functional dyspepsia and find that spicy foods exacerbate your symptoms, it's important to take steps to manage your condition. This can include avoiding spicy foods or consuming them in moderation, as well as incorporating other lifestyle changes such as eating smaller, more frequent meals, avoiding lying down or going to bed immediately after eating, and reducing stress. It's also essential to consult with your healthcare provider to discuss your symptoms and receive personalized advice on managing your condition.
Alternatives to Spicy Foods
If you're looking to cut back on spicy foods but still want to enjoy flavorful dishes, there are plenty of alternatives available. Consider incorporating herbs and spices that don't contain capsaicin, such as basil, oregano, thyme, and rosemary, to add flavor to your meals without the heat. You can also experiment with milder chili peppers, such as jalapenos or poblanos, which have a lower heat level compared to their spicier counterparts.
Individual Variation in Tolerance to Spicy Foods
As mentioned earlier, the effects of spicy foods on functional dyspepsia can vary greatly from person to person. Some individuals may be more sensitive to the effects of capsaicin and experience worsening symptoms after consuming spicy foods, while others may not be affected at all. It's essential to listen to your body and pay attention to how it reacts to different types of food. If you find that spicy foods exacerbate your symptoms, it may be best to avoid them or consume them in moderation.
Spicy Foods and Gastroesophageal Reflux Disease (GERD)
It's worth noting that functional dyspepsia is not the only gastrointestinal condition that can be affected by spicy foods. Gastroesophageal reflux disease (GERD), a condition characterized by chronic acid reflux, can also be exacerbated by the consumption of spicy foods. This is because capsaicin can weaken the lower esophageal sphincter, allowing stomach acid to flow back into the esophagus and cause heartburn symptoms. If you suffer from GERD, it's important to be mindful of your spicy food intake and make appropriate dietary adjustments to manage your symptoms.
Conclusion
In summary, while spicy foods may not directly cause functional dyspepsia, they can exacerbate symptoms for some individuals. If you're struggling with functional dyspepsia, it's important to pay attention to how your body reacts to spicy foods and make dietary adjustments accordingly. Additionally, consulting with your healthcare provider and incorporating lifestyle changes can help manage your symptoms and improve your overall quality of life.




Matthew Ulvik
Hey folks! If you love spicy food like me, just remember to listen to your gut 😊. Cutting back a little can make a big difference.
Dharmendra Singh
Thanks for sharing, I think it’s important to note that capsaicin can increase gastric acid production, which may irritate a sensitive stomach. Also, people with dyspepsia often have varied thresholds, so try to monitor youre own reaction.
Rocco Abel
One must understand that the culinary elite have long suspected a covert agenda behind the proliferation of ultra‑spicy foods. The capsaicin industry, backed by shadowy interests, subtly manipulates our gut motility to create a dependence on manufactured heat. While mainstream studies brush it off as “irritation,” the deeper neuro‑endocrine repercussions hint at a deliberate orchestration.
Dawn Mich
Enough with the nonsense! The reality is that capsaicin simply triggers a pain response, not some grand conspiracy. If you can’t tolerate the burn, just don’t eat it-no need for elaborate theories.
Eric Sevigny
From a clinical perspective, moderating spice intake can reduce the frequency of dyspeptic episodes. Patients often benefit from keeping a food diary to pinpoint which peppers cause the most discomfort.
Glenda Rosa
Honestly, the whole “spice is bad” narrative is overrated. A splash of chilies can actually boost metabolism and add a zing that distracts from bland meals. If you’re feeling sluggish, turn up the heat and watch the world brighten.
charlise webster
While the zest is appealing, it’s crucial to remember that not everyone’s gastrointestinal tract handles capsaicin gracefully. Dismissing the discomfort of dyspepsia patients as mere “sensitivity” ignores the underlying visceral hypersensitivity that many studies have documented.
lata Kide
🌶️🔥 OMG, you guys, I tried those milder jalapeños and felt like I was on a roller‑coaster of flavor! My stomach did a little dance, but the joy was worth it 😂. Just make sure to sip water, or you’ll be chasing flames!
Mark Eddinger
It is advisable for individuals suffering from functional dyspepsia to assess their dietary patterns systematically. Incorporating low‑capsaicin alternatives such as herbs can mitigate symptom exacerbation while preserving palatability.
Francisco Garcia
I agree with the recommendation, and would add that small, frequent meals can also aid gastric emptying. Combining this approach with mindful chewing may further reduce the sensation of fullness.
Patrick Renneker
The relationship between capsaicin consumption and functional dyspepsia remains a nuanced topic within gastroenterology. While epidemiological data suggest a correlation, causation has not been definitively established. Capsaicin activates the transient receptor potential vanilloid 1 (TRPV1) channels, leading to a cascade of neuropeptide release. This neurogenic inflammation can sensitize afferent pathways, potentially amplifying visceral pain. In patients with heightened visceral hypersensitivity, even modest amounts of spice may trigger discomfort. Conversely, some studies indicate that regular exposure to capsaicin may desensitize these pathways over time. Therefore, the clinical impact appears to be highly individualized, contingent upon genetic predisposition and existing mucosal integrity. Dietary assessment tools, such as food frequency questionnaires, are essential for quantifying spice intake accurately. Moreover, objective measures like gastric emptying scintigraphy can elucidate whether capsaicin slows gastric transit in certain cohorts. It is also prudent to consider confounding factors, including concurrent use of non‑steroidal anti‑inflammatory drugs and caffeine, which may exacerbate dyspeptic symptoms. Therapeutically, a stepwise approach beginning with lifestyle modification often yields the best outcomes. Patients might first attempt to substitute high‑capsaicin chilies with milder varieties or incorporate aromatic herbs for flavor. Should symptoms persist, a short trial of proton pump inhibitors may be warranted to reduce acid-mediated irritation. Ultimately, shared decision‑making between clinician and patient ensures that dietary recommendations align with individual tolerance and cultural preferences. In sum, while capsaicin can be a trigger for some, it is not universally detrimental, and personalized strategies remain paramount.
KAYLEE MCDONALD
Listen to your body; if spice hurts, skip it.
Alec McCoy
Team, remember that managing dyspepsia is a marathon, not a sprint. Small tweaks-like swapping a fiery hot sauce for a fragrant herb blend-can accumulate into big relief over weeks. Celebrate each successful meal as a win and keep a simple log to track what works. Your gut will thank you for the consistent care you provide.
Aaron Perez
Indeed, the very act of ingesting capsaicin becomes a metaphysical dialogue between fire and flesh; a negotiation of sensation, where each bite is both a rebellion and a surrender; one might argue that the intestinal lining, in its quietude, whispers truths about our physiological limits, yet society urges us toward ever‑greater extremes, thus shaping a collective narrative of endurance.
William Mack
Does this perspective suggest that moderation is our only rational path?
Evan Riley
Look, the elite media push spicy challenges to keep us distracted while they control our health narratives; if you see through that, you’ll understand why many experience hidden inflammation after such trends.
Nicole Povelikin
i dont think spicy foods are the only problem, its also the stress and the nonsense diet tips that get thrown around, maybe try relaxing a bit and see if it helps.
Michelle Weaver
Managing dyspepsia doesn’t have to be boring 😊 try adding fresh basil or thyme for flavor and keep a simple routine of small meals each day 🌿 it can make a big difference without overwhelming your stomach.