Introduction: Understanding Crohn's Disease and Gluten Intolerance
Crohn's disease and gluten intolerance are two conditions that can significantly impact a person's quality of life. Both conditions can cause similar symptoms and often lead to confusion about their true cause. In this article, we will dive into the link between these two conditions and provide some helpful information on what to watch for if you suspect you may be suffering from one or both of them.
Overview of Crohn's Disease
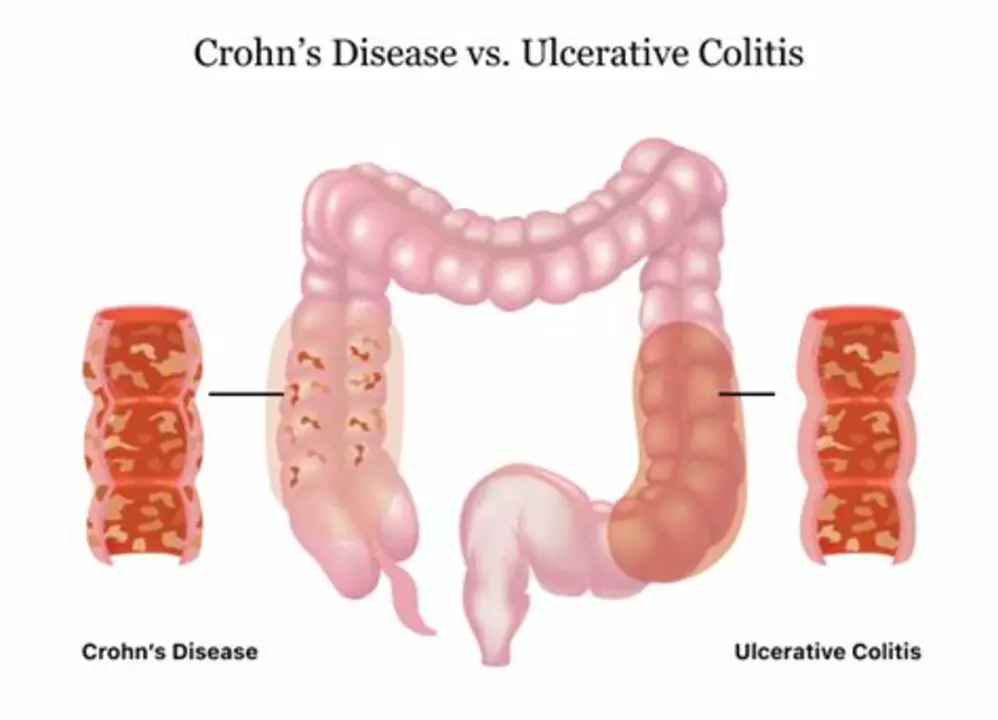
Crohn's disease is a type of inflammatory bowel disease (IBD) that affects the gastrointestinal tract. It can cause inflammation and damage to any part of the GI tract, from the mouth to the anus, though it most commonly affects the small intestine and the beginning of the large intestine. The exact cause of Crohn's disease is unknown, but it is believed to be a combination of genetic, environmental, and immune system factors.
Overview of Gluten Intolerance
Gluten intolerance, also known as non-celiac gluten sensitivity (NCGS), is a condition in which individuals experience symptoms similar to those of celiac disease but do not test positive for the condition. These symptoms can include abdominal pain, bloating, diarrhea, and fatigue. Unlike celiac disease, which is an autoimmune disorder, gluten intolerance is not well understood and there is no definitive test for it. However, eliminating gluten from the diet often leads to symptom relief for those who are intolerant.
The Connection Between Crohn's Disease and Gluten Intolerance
While Crohn's disease and gluten intolerance are separate conditions, there is evidence to suggest that they may be connected in some cases. Some studies have found that individuals with Crohn's disease are more likely to have gluten sensitivity than the general population. Additionally, those with gluten intolerance may be at a higher risk of developing Crohn's disease due to the inflammation caused by their immune system's response to gluten.
Common Symptoms Shared by Both Conditions
Both Crohn's disease and gluten intolerance can cause a variety of gastrointestinal symptoms, including abdominal pain, bloating, diarrhea, and constipation. They can also cause non-GI symptoms such as fatigue, joint pain, and skin rashes. Because of these similarities, it can be difficult to determine which condition is responsible for a person's symptoms without proper testing and evaluation.
Testing and Diagnosis: Differentiating Between Crohn's Disease and Gluten Intolerance
Diagnosing Crohn's disease typically involves a combination of blood tests, imaging studies, and endoscopic procedures to evaluate the GI tract. In contrast, diagnosing gluten intolerance can be more challenging, as there is no definitive test for the condition. A trial of a gluten-free diet is often used to determine if an individual's symptoms improve without gluten.
When to Consult a Healthcare Professional
If you are experiencing persistent gastrointestinal symptoms that are impacting your daily life, it is important to consult with a healthcare professional. They can help determine the cause of your symptoms and recommend appropriate tests and treatments. Early intervention can help minimize complications and improve your quality of life.
Treatment and Management of Crohn's Disease
Treatment for Crohn's disease typically involves a combination of medications, dietary modifications, and lifestyle changes. Medications may include anti-inflammatory drugs, immunosuppressants, and biologic therapies to help control inflammation and prevent complications. Dietary modifications may include avoiding trigger foods, such as high-fat or high-fiber foods, and consuming smaller, more frequent meals. Regular exercise, stress management, and adequate sleep are also important components of managing Crohn's disease.
Treatment and Management of Gluten Intolerance
The primary treatment for gluten intolerance is a strict gluten-free diet, which involves eliminating all sources of gluten from the diet. This includes avoiding wheat, barley, rye, and any products containing these grains. It is also important to be aware of hidden sources of gluten in processed foods and medications. In addition to dietary changes, individuals with gluten intolerance may benefit from nutritional supplements to address any nutrient deficiencies resulting from their restricted diet.
Conclusion: Navigating the Complexities of Crohn's Disease and Gluten Intolerance
Understanding the link between Crohn's disease and gluten intolerance is crucial for those who suffer from these conditions. By recognizing the similarities and differences between these two conditions, individuals can work with their healthcare providers to develop a comprehensive treatment plan that addresses their unique needs. With proper management, many people with Crohn's disease and gluten intolerance can lead healthy, fulfilling lives.




Abigail Lynch
Just read this and I can’t help but wonder why Big Pharma isn’t shouting from the rooftops about the hidden gluten link – they’re probably scared we’ll finally catch on to their secret agenda.
David McClone
Oh sure, because the next step is clearly a gluten‑free vaccine that will also cure my chronic sarcasm – color me impressed.
Jessica Romero
From a gastroenterological perspective, the pathophysiology of Crohn’s disease involves a dysregulated immune response characterized by Th1/Th17 cytokine profiles, which can be exacerbated by antigenic stimuli such as gluten peptides.
When gluten enters the lumen of a genetically predisposed individual, it may trigger zonulin-mediated tight‑junction modulation, increasing intestinal permeability and facilitating translocation of bacterial endotoxins.
This leaky gut phenomenon can amplify the mucosal immune activation already present in Crohn’s, creating a feedback loop of inflammation.
Moreover, studies employing ELISA assays have demonstrated elevated IgG anti‑gliadin antibodies in a subset of Crohn’s patients, suggesting serological overlap.
Endoscopic biopsies sometimes reveal villous blunting reminiscent of celiac disease, yet the histological hallmark of granulomas remains distinct for Crohn’s.
The clinical overlap-abdominal pain, chronic diarrhea, weight loss-poses diagnostic challenges, especially when patients self‑implement a gluten‑free diet before proper work‑up.
In practice, a structured elimination trial, typically spanning 6–8 weeks, coupled with validated symptom scoring, can elucidate gluten’s role without confounding factors.
Nonetheless, clinicians must remain vigilant for nutritional deficiencies that may arise from unnecessary dietary restrictions, such as iron, B12, and folate deficits.
From a therapeutic standpoint, biologics targeting TNF‑α or integrin pathways do not directly address gluten‑induced mechanisms, but they can reduce overall inflammatory burden, potentially mitigating gluten sensitivity symptoms.
Conversely, dietary interventions-low‑FODMAP, exclusive elemental formulas-are adjuncts that can be tailored based on patient response.
It is also worth noting that microbiome dysbiosis, a common feature in both Crohn’s and non‑celiac gluten sensitivity, may act as a confounding variable, influencing symptom perception and immune modulation.
Metagenomic sequencing has revealed reduced Bifidobacterium and increased Proteobacteria in both cohorts, suggesting a shared microbial signature that could be targeted with probiotic or prebiotic strategies.
Therefore, the intersection of Crohn’s disease and gluten intolerance is multifactorial, encompassing immunogenetics, barrier function, microbiota, and dietary patterns.
Future research employing longitudinal cohort studies with standardized gluten challenges and multi‑omics profiling will be essential to delineate causality versus correlation.
In summary, clinicians should adopt a comprehensive, patient‑centered approach that integrates serology, endoscopy, dietary trials, and emerging biomarker data to properly differentiate and manage these overlapping conditions.
Michele Radford
Honestly, people who think they can just blame everything on gluten are shirking responsibility and feeding a culture of victimhood that undermines real medical science.
Mangal DUTT Sharma
I totally feel you 🙏-dealing with these gut issues can be a rollercoaster, but remember you’re not alone, and a supportive community can make the journey a bit brighter 😊.
Gracee Taylor
It’s great to see everyone sharing insights; I think the key is to stay open‑minded and work with a doctor you trust to find what works for you personally.
Leslie Woods
What are the main signs that differentiate Crohn’s from gluten sensitivity also how long should a gluten free trial be
Manish Singh
i think its importent to listen to the body its often tell us wht is wrong but many times we ignore it i have seen ppl do the same with diet changes and end up feeling worse
Dipak Pawar
From a cultural health perspective, many South Asian diets are already low in wheat and barley, which unintentionally creates a quasi‑gluten‑free environment; however, rice‑based staples can be high in FODMAPs, potentially exacerbating IBS‑like symptoms in susceptible individuals. It’s fascinating how regional culinary practices intersect with modern biomedical understandings of gut health, and it reminds clinicians to consider ethnographic dietary patterns when evaluating patients for gluten sensitivity versus inflammatory bowel disease.
Jonathan Alvarenga
Reading this feels like watching a low‑budget infomercial-lots of hype, no solid proof, just a convenient excuse for people to avoid carbs and feel superior.
Jim McDermott
Wow, that thorough breakdown really helped me see how many layers there are-especially the part about microbiome overlap, which I hadn’t considered before. I’m thinking of discussing a gluten trial with my gastroenterologist to see if it eases some of my flare‑ups.
Naomi Ho
If you decide to try a gluten‑free elimination, aim for at least six weeks and keep a simple symptom diary-note stool consistency, abdominal pain, and energy levels daily. This data will give your doctor a clear picture and help avoid vague conclusions.