Not all joint pain is the same
If you’ve been told you have arthritis, the first thing you need to know is this: osteoarthritis and rheumatoid arthritis are not the same condition. They don’t start the same way, they don’t feel the same, and they sure as heck aren’t treated the same. Yet so many people mix them up - and that can cost you time, mobility, and even your future joint health.
Let’s cut through the noise. This isn’t about medical jargon. It’s about knowing what’s actually happening in your body when your knees ache, your fingers stiffen, or you wake up feeling like you’ve been hit by a truck.
Osteoarthritis: The Wear-and-Tear Type
Osteoarthritis, or OA, is what happens when the cushion between your bones - the cartilage - slowly breaks down. Think of it like the rubber on your shoe heels wearing thin after years of walking. It’s not an infection. It’s not your immune system attacking you. It’s just mechanics. Over time, the joint loses its smooth surface. Bone starts rubbing on bone. That’s when pain, grinding, and swelling show up.
It usually hits the joints that carry weight or get used a lot: knees, hips, lower back, and the ends of your fingers. You’ll notice it more after standing all day, walking far, or lifting something heavy. Rest usually helps. Morning stiffness? It’s there, but it lasts less than 30 minutes. That’s a big clue.
Age is the biggest risk factor. Most people start seeing signs after 50. But it’s not just age. If you’ve had a knee injury, worked a physically demanding job, or carry extra weight, your risk shoots up. Studies show losing just 5kg can cut knee OA pain by half. That’s not a guess - it’s from real clinical data.
On an X-ray, OA shows up as narrowing joint space and little bone spurs sticking out like tiny spikes. There’s no blood test for it. Doctors diagnose it by looking at your symptoms, how your joint moves, and what the images show.
Rheumatoid Arthritis: The Body Turns on Itself
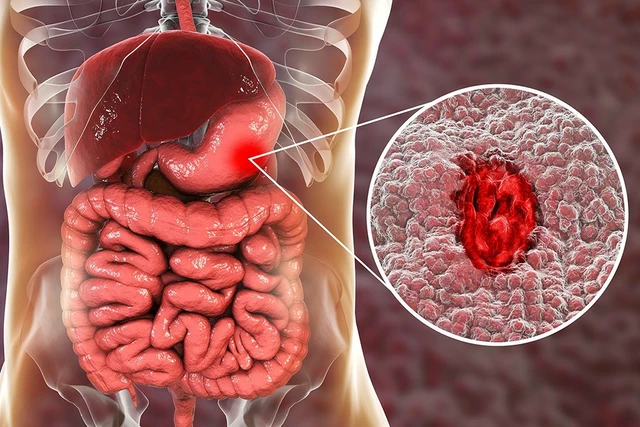
Rheumatoid arthritis (RA) is a different beast entirely. This isn’t wear and tear. This is your immune system going rogue. It mistakes the lining of your joints - the synovium - for a threat and starts attacking it. That triggers inflammation, swelling, heat, and pain. Left unchecked, it doesn’t just hurt your joints. It can destroy cartilage, erode bone, and damage tendons.
RA doesn’t wait until you’re old. It can strike in your 30s, 40s, even late teens. And it doesn’t pick one side. It hits both wrists, both knees, both hands - symmetrical, like a mirror image. That’s a dead giveaway.
Morning stiffness? That’s one of the biggest signs. You might feel locked up for over an hour. Not just stiff - exhausted. Fatigue, low fevers, even weight loss can come with it. RA doesn’t stay in the joints. It can affect your lungs, heart, eyes, and skin. Some people get hard lumps under the skin near their elbows - rheumatoid nodules. You won’t see those with OA.
Doctors look for two key blood markers: rheumatoid factor (RF) and anti-CCP antibodies. These aren’t perfect, but when they’re high and symptoms match, it’s strong evidence. Ultrasound and MRI can catch early inflammation before X-rays show damage. That’s why early diagnosis matters. If you wait too long, joint damage can become permanent within months.
And here’s the hard truth: OA can be managed. RA must be treated aggressively. Delayed treatment means irreversible damage. That’s why seeing a rheumatologist fast is non-negotiable if RA is suspected.

Other Common Types of Arthritis You Should Know
OA and RA make up the bulk of cases, but they’re not the whole story.
Psoriatic arthritis shows up in people with psoriasis - that scaly skin condition. It often affects fingers and toes, sometimes making them swell up like sausages. It can also hurt your spine and cause nail changes. Like RA, it’s autoimmune.
Gout is sudden, brutal pain, usually in the big toe. It happens when uric acid crystals build up in the joint. One minute you’re fine, the next you can’t put your foot down. Attacks come and go, but without lifestyle changes, they get worse. Diet plays a big role - red meat, alcohol, sugary drinks can trigger it.
Ankylosing spondylitis targets the spine and pelvis. It starts with lower back pain that’s worse in the morning and improves with movement. Over time, it can fuse vertebrae together. It often runs in families and shows up in young men more than women.
Juvenile idiopathic arthritis affects kids under 16. It’s not just growing pains. It can cause fever, rash, swollen joints, and even eye inflammation. Early treatment is critical to prevent lifelong issues.
How Diagnosis Works - What Tests Really Tell You
Doctors don’t guess. They piece things together.
For OA: physical exam, X-ray, and your history. Blood tests usually come back normal. If they’re abnormal, it’s probably not OA.
For RA: blood tests for RF and anti-CCP, plus imaging. Inflammation markers like CRP and ESR often spike. Ultrasound can show swelling in the synovium before bones get damaged.
For gout: joint fluid test. A needle pulls out fluid, and if you see uric acid crystals under the microscope? That’s it.
For psoriatic arthritis: look for psoriasis on skin or nails, plus imaging. Blood tests might be normal, so diagnosis relies on pattern recognition.
Don’t rely on one test. It’s the full picture - symptoms, timing, exam, and tests - that gives the answer.
Treatment: Why You Can’t Swap One for the Other
This is where people get hurt.
OA treatment is about reducing stress on the joint and managing pain. Lose weight. Move regularly - swimming and cycling are great. Physical therapy strengthens muscles around the joint. NSAIDs like ibuprofen help with pain and swelling. Injections of corticosteroids or even PRP (platelet-rich plasma) are options, though evidence for PRP is still mixed. When everything else fails, joint replacement surgery works wonders - and 90% of all joint replacements in the U.S. are for OA.
RA treatment is completely different. You don’t just treat the pain. You stop the immune system from destroying your joints. That means DMARDs - disease-modifying drugs like methotrexate. These take weeks to work, but they change the course of the disease. If DMARDs aren’t enough, biologics - targeted drugs like Humira or Enbrel - come in. These are expensive, sometimes $20,000 to $50,000 a year, but they can put RA into remission. JAK inhibitors like tofacitinib are newer options. The goal? Stop inflammation before it ruins your joints.
Here’s the bottom line: If you have RA and get OA treatment, you’re leaving the fire burning. If you have OA and get RA drugs, you’re exposing yourself to serious side effects for no benefit. Misdiagnosis isn’t just a mistake - it’s dangerous.

Who’s at Risk? The Real Factors Behind the Pain
OA isn’t just ‘getting old.’ It’s linked to:
- Obesity (BMI over 30 increases knee OA risk by 4.5 times)
- Previous joint injury
- Repetitive stress from work or sports
- Genetics - if your mom had hand OA, you’re more likely to
RA risk factors are different:
- Smoking - doubles or triples your risk
- Family history - especially HLA-DRB1 gene variants
- Gender - women are 2 to 3 times more likely to get it
- Environmental triggers - like silica dust or certain infections
And yes, some studies suggest RA is more common in Black populations, while OA is higher in white populations - but this isn’t settled science. What’s clear is that lifestyle and genetics interact in complex ways.
What’s New in 2025?
Science is moving fast.
For RA, new biologics and JAK inhibitors are becoming safer and more targeted. The focus now is on remission - not just slowing damage, but stopping it completely. Studies show 30% to 50% of patients can reach remission with early, aggressive treatment.
For OA, researchers are hunting for blood or urine biomarkers that detect cartilage breakdown before X-rays show anything. That could mean catching it years earlier. PRP and stem cell injections are still being studied, but they’re not magic bullets - yet.
Ultrasound is now part of the standard RA workup, not just an add-on. And guidelines from the American College of Rheumatology now push for diagnosis and treatment within the first 3 to 6 months of symptoms. That window is everything.
Bottom Line: Know Your Arthritis
If your joints hurt, don’t just accept it as ‘normal aging.’ Ask: Is this wear and tear? Or is something deeper going on?
Ask yourself:
- Is the pain worse after activity and better with rest? → Likely OA.
- Do both sides of your body hurt the same? Is morning stiffness over an hour? Are you tired, feverish, or losing weight? → Think RA.
- Did the pain come on suddenly in one joint, especially the big toe? → Could be gout.
Don’t wait. See a doctor. Get the right tests. If RA is possible, don’t delay - see a rheumatologist. Early action can keep you walking, working, and living without pain.
This isn’t just about pain relief. It’s about protecting your future.
Can you have both osteoarthritis and rheumatoid arthritis at the same time?
Yes. It’s not common, but it happens. Someone might develop OA in their knees from years of running, then later develop RA due to autoimmune triggers. The symptoms can overlap, which makes diagnosis tricky. That’s why blood tests and imaging are essential - to separate the wear-and-tear damage from active inflammation.
Does weather really affect arthritis pain?
Many people swear their joints ache when it’s cold or damp. Studies show a small but real link between barometric pressure changes and increased pain - especially in OA. It’s not the cause, but it can make existing pain feel worse. Staying warm, moving gently, and using heat packs can help.
Is arthritis curable?
Osteoarthritis isn’t curable - but it’s manageable. You can slow it down and live well. Rheumatoid arthritis isn’t curable either, but modern treatments can put it into remission. That means no pain, no swelling, no damage - for years, sometimes decades. The goal isn’t a cure. It’s control.
Can diet help with arthritis?
For OA, losing weight is the single most effective dietary step. For RA, anti-inflammatory foods - like fatty fish, leafy greens, nuts, and berries - may help reduce flares. Avoiding sugar, processed foods, and excess alcohol helps everyone. Gout? Cut back on red meat, shellfish, and beer. Diet won’t cure arthritis, but it can make a real difference in how you feel.
Should I stop exercising if my joints hurt?
No - but change how you move. High-impact activities like running can worsen OA. Switch to swimming, cycling, or tai chi. For RA, gentle movement keeps joints flexible and muscles strong. In fact, staying active is one of the best ways to reduce pain and stiffness. A physical therapist can help you find safe exercises tailored to your type of arthritis.




Michael Dioso
Let me stop you right there. Osteoarthritis isn't just 'wear and tear' - that's what they taught you in med school 20 years ago. Modern studies show it's inflammatory at the molecular level too. Cartilage isn't just eroding - it's actively being broken down by cytokines. You're selling people a myth if you think it's purely mechanical. And don't get me started on PRP - half the clinics are scamming people with placebo injections.
Rupa DasGupta
I had RA since I was 22 and they told me it was just 'overuse' for 3 years 😭 I lost my job, my marriage, my dignity... then one doc finally saw the nodules and said 'this ain't aging, this is war.' Now I'm on biologics and I can hold my baby again. 🤍 Please don't ignore morning stiffness - it's not laziness, it's your body screaming.
Marvin Gordon
This is the clearest breakdown I've ever seen. Seriously. I've been dealing with knee pain for 5 years and thought it was just 'getting old.' Now I know it's OA, and I'm finally losing weight and hitting the pool. No more excuses. If you're reading this and hurting - move. Even a little. Your future self will thank you.
ashlie perry
They don't want you to know this but the FDA is hiding the truth about RA drugs. Big Pharma makes billions off biologics. The real cause? 5G towers + glyphosate in your food. I know a guy who cured his arthritis with Himalayan salt and moonlight. You think your blood test means anything when the system is rigged?
Ali Bradshaw
I'm a physio in Glasgow and I see this every day. People with OA think rest is the answer. It's not. Movement is medicine. Even gentle cycling or water aerobics keeps the synovial fluid flowing. I've had patients go from canes to hiking trails in 6 months. Don't give up. Your joints aren't broken - they're just neglected.
an mo
The data is clear: RA prevalence in white females is statistically significant (p<0.001) due to HLA-DRB1*04 allele expression. The 2.3x higher incidence isn't anecdotal - it's a genetic epidemiological fact. Meanwhile, OA disparities in non-Caucasian populations are confounded by socioeconomic access to diagnostics. You're misrepresenting the data by implying racial causality without controlling for healthcare access.
aditya dixit
There's a quiet truth here: arthritis is not just a disease of the body, but of the soul. When we treat it as a mechanical failure, we forget that pain is a messenger. OA teaches patience. RA teaches surrender. Gout teaches humility. And perhaps the greatest lesson? We are not separate from our bodies - we are our bodies. To heal is to listen, not just to treat.
William Chin
I must respectfully submit that the assertion that 'OA is not an autoimmune condition' requires immediate revision in light of recent peer-reviewed findings published in Nature Rheumatology (2024), wherein IL-17A-mediated synovial inflammation was observed in 68% of OA patients with radiographic progression. To categorically dismiss systemic inflammation in OA is not only scientifically inaccurate, it is clinically irresponsible.
Ada Maklagina
I got both OA and RA and honestly the worst part isn't the pain it's the doctors who act like you're lying when you say both hurt