Gene Therapy Drug Interaction Checker
Medication Input
Enter all medications you take before gene therapy treatment
Interaction Results
Key Risks to Understand
Immune response: Viral vectors can trigger inflammation that changes liver enzyme function (CYP3A4, CYP2C9), leading to unexpected drug levels.
Long-term monitoring: Interactions may develop months or years after treatment. Never adjust medications without consulting your care team.
Enter your medications to see potential interactions
Gene therapy isn’t just another new drug. It’s a one-time treatment that changes your DNA to fix a broken gene. Sounds like science fiction? It’s real. And it’s changing how we treat inherited diseases like sickle cell anemia, certain forms of blindness, and rare metabolic disorders. But here’s the catch: once you get it, your body doesn’t just accept it quietly. It reacts. And those reactions can interfere with every other medication you’re taking-sometimes in ways no one predicted.
Why Gene Therapy Is Different From Regular Drugs
Most drugs work like keys turning locks. They bind to proteins, block signals, or boost activity. They’re temporary. You take them daily or weekly. They leave your system. Gene therapy is permanent. It delivers new genetic instructions into your cells-often using modified viruses as delivery trucks. These viruses aren’t meant to make you sick, but they still look like invaders to your immune system. That’s where things get dangerous. In 1999, an 18-year-old named Jesse Gelsinger died after receiving gene therapy for a rare liver disorder. His body mounted a massive immune response to the adenovirus vector used to carry the gene. His liver failed. His organs shut down. He wasn’t the first to die in a gene therapy trial, but he was the first whose death forced the world to pay attention. Since then, we’ve learned that these viral vectors don’t just trigger immune reactions. They can slip into the wrong parts of your DNA. In early trials for severe immune deficiencies, the therapy accidentally activated cancer-causing genes. Five children developed leukemia. One died. The vector had landed right next to a gene called LMO2, flipping it on like a switch. That’s not a side effect. That’s a rewrite.How Gene Therapy Messes With Your Medications
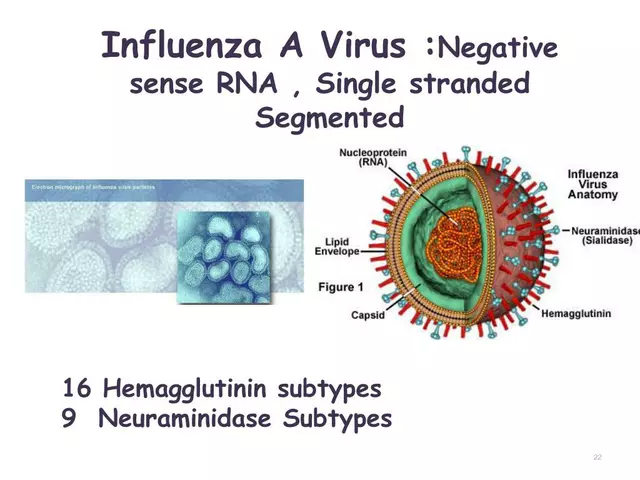
Your body uses enzymes-mostly from the CYP450 family-to break down most prescription drugs. Statins. Antidepressants. Blood thinners. Even common painkillers. These enzymes are like your body’s detox machines. And gene therapy can turn them up, turn them down, or break them entirely. When a viral vector enters your bloodstream, your immune system goes on high alert. Inflammatory signals flood your liver. That’s where most drug metabolism happens. Suddenly, your CYP3A4 enzyme-the one that handles nearly half of all medications-starts working faster or slower. Your blood levels of warfarin might drop, putting you at risk for clots. Or your statin might build up, causing muscle damage. You don’t know until it’s too late. And it’s not just the immune system. The therapy itself can change how your cells behave. If the gene therapy makes your liver cells produce more of a protein that breaks down drugs, your antidepressant might stop working. If it alters your kidney function, your blood pressure meds could become toxic. There are no warning labels for this. No drug interaction charts in the medical textbooks. Because until recently, these interactions didn’t exist.Off-Target Effects: When the Therapy Hits the Wrong Cells
Gene therapy is supposed to target specific tissues-liver, retina, muscle. But viruses don’t always obey. Adeno-associated viruses (AAVs), now the most common delivery tool, can end up in your heart, your brain, or your spleen. That’s not always bad. But if those cells start producing the new gene product, you get side effects no one planned for. Imagine a therapy meant to fix a muscle disorder. The virus ends up in your pancreas. Now your pancreas starts making a growth factor it never should. That could trigger abnormal cell growth. Or worse-cancer. This isn’t theoretical. Animal studies show it happens. Human data is still emerging, but we’ve seen cases where gene therapy led to tumors years later. And then there’s the problem of transplanted cells. Some gene therapies involve removing your blood stem cells, editing them in the lab, and putting them back. What if one of those edited cells turns cancerous? It could spread. And if it does, your immune system might not recognize it as foreign. Your chemo drugs? They might not work. Your immunotherapy? It might overreact.
Long-Term Monitoring Isn’t Optional-It’s Mandatory
Regular drugs are monitored for 30 days. Gene therapy? The FDA requires 15 years of follow-up for therapies that integrate into your DNA. Why? Because some risks don’t show up for years. A child gets gene therapy for a rare disease at age 5. Ten years later, they develop a brain tumor. Was it the therapy? The environment? Genetics? No one knows. But without long-term tracking, we’ll never find out. That’s why doctors now track patients for life. Blood tests. MRI scans. Genetic screenings. Even if the patient feels fine. Even if they’ve stopped seeing their specialist. The risk doesn’t disappear after six months. It just hides. And here’s the kicker: if you’re on long-term medication-say, for epilepsy or heart disease-and you get gene therapy, your drug regimen might need to change. Not tomorrow. Not next year. Maybe in five. But you’ll need to know.Viral Transmission: The Hidden Risk to Family Members
You might think gene therapy only affects you. But some vectors can be shed. Through saliva, urine, or even semen. The FDA now requires companies to prove their therapies won’t spread to family members. But what if they do? Imagine a father gets gene therapy for a liver condition. A week later, his toddler kisses him on the cheek. The virus from his saliva enters the child’s body. The child wasn’t consented. Wasn’t tested. Isn’t being monitored. Now they’ve been exposed to a genetic treatment they never agreed to-and could develop side effects years later. This isn’t science fiction. It happened in early trials. A child developed antibodies to the vector after being exposed to their sibling’s bodily fluids. No symptoms. No immediate danger. But now, if that child ever needs gene therapy themselves, the treatment won’t work. Their immune system will attack it.
What Doctors Don’t Know Yet
We’re flying blind in a lot of ways. There’s no database that tracks which gene therapies interact with which drugs. No algorithm predicts how a patient’s genetic background will affect their response. We don’t even know how common these interactions are. A 2023 study in Nature Medicine found that 42% of patients in gene therapy trials were taking at least one medication known to interact with immune pathways. Yet only 3 of those 100 patients had their drug doses adjusted. No one checked for changes in liver enzyme activity. No one looked at drug levels in the blood. And genetic diversity? We’re still mostly testing on people of European descent. But gene therapy responses vary wildly across populations. A variant in the CYP2D6 gene, common in East Asians, can make someone a super-metabolizer-or a poor one. That changes how they handle every drug they take. We don’t know how gene therapy interacts with those variants.What You Need to Do If You’re Considering Gene Therapy
If you or a loved one is being considered for gene therapy, here’s what you need to do:- List every medication you take-prescription, over-the-counter, supplements, even herbal remedies. Don’t leave anything out.
- Ask your doctor: "Will this gene therapy affect how my other drugs work?" If they don’t know, ask for a pharmacogenomics consultation.
- Understand the long-term plan: Who will monitor you? For how long? What tests will be done? When?
- Know the risks of transmission: If you’re on a therapy that sheds, avoid close contact with infants, pregnant people, or immunocompromised individuals for at least a month.
- Keep a personal record: Write down every drug you take before and after therapy. Note any new symptoms-fatigue, rashes, mood changes, unexplained pain. These could be early signs of an interaction.
Gene therapy is powerful. It can give people back their sight. It can cure diseases that once meant early death. But it’s not magic. It’s biology. And biology doesn’t care about our hopes. It follows its own rules. We’re still learning them.
Can gene therapy interact with over-the-counter drugs like ibuprofen or vitamin supplements?
Yes. Even common painkillers like ibuprofen or supplements like fish oil can interact with gene therapy. The immune response triggered by the viral vector can change how your liver processes these substances. Ibuprofen, for example, is metabolized by CYP2C9-a pathway that can be suppressed or boosted after gene therapy. This can lead to unexpected bleeding, stomach ulcers, or reduced effectiveness. Always disclose every supplement and OTC drug to your care team before treatment.
How long should I wait before starting a new medication after gene therapy?
There’s no universal timeline. Some patients can resume medications within weeks. Others need to wait six months or longer. It depends on the vector used, the target tissue, and your immune response. Your medical team should monitor your liver enzymes and drug levels through blood tests before restarting any new medication. Never start a new drug without their approval.
Are there any drugs I should avoid completely after gene therapy?
Some drugs carry higher risks. Immunosuppressants like prednisone can mask dangerous immune reactions to the vector, delaying diagnosis. Chemotherapy drugs can increase the chance of cancer if the therapy has already altered your DNA. Blood thinners like warfarin require extremely careful monitoring because gene therapy can unpredictably change how your body metabolizes them. Always consult a pharmacogenomics specialist before taking any new drug.
Can gene therapy affect how my birth control works?
Yes. Hormonal contraceptives are metabolized by CYP3A4, an enzyme often affected by gene therapy. If your liver starts breaking down the hormones faster, your birth control could become ineffective. If it slows down, you could experience side effects like blood clots. If you’re on gene therapy, use non-hormonal contraception (like an IUD) until your care team confirms your hormone levels are stable.
What happens if I need emergency surgery after gene therapy?
Emergency surgery is high-risk. Anesthesia drugs, painkillers, and antibiotics are all metabolized by the liver. If your gene therapy altered your enzyme activity, standard doses could be too strong or too weak. Always carry a medical alert card or digital record listing your gene therapy, the vector used, and your treating center’s contact info. Inform every healthcare provider-even paramedics-before any procedure.




Glenda Walsh
Wait, so if I get this therapy, my ibuprofen might suddenly turn into a blood thinner?? And my fish oil could make me bleed out?? I just took two Advil before bed-AM I IN DANGER??
Raj Modi
It is imperative to recognize that the introduction of gene therapy into the clinical domain represents not merely a therapeutic innovation, but a paradigmatic shift in the relationship between the human organism and exogenous biological agents. The viral vectors employed, while engineered for specificity, retain inherent immunogenic properties that interact unpredictably with the host’s metabolic enzymatic machinery, particularly the cytochrome P450 system. Consequently, the pharmacokinetic profiles of concomitant medications-ranging from anticoagulants to psychotropics-may undergo profound, non-linear alterations, rendering standard dosing protocols obsolete. This necessitates a multidisciplinary approach involving pharmacogenomic specialists, hepatologists, and immunologists to ensure patient safety over the long term.
Cecil Mays
Bro this is wild 🤯 I had no idea my vitamin D supplement could turn into a landmine after gene therapy. But seriously-this is why we need more people like you sharing this stuff. My cousin just got treated for sickle cell and no one told her about the drug stuff. Please, someone make a simple infographic for this. 🙏 #GeneTherapyAwareness
Sarah Schmidt
Of course the medical establishment is flying blind. They’ve spent decades treating symptoms while ignoring root causes-now they’ve weaponized biology and wonder why chaos follows. This isn’t medicine. It’s alchemy with a FDA stamp. You think they care about your warfarin levels? They care about stock prices and patent expiration dates. You’re not a patient-you’re a data point in a billion-dollar experiment. And you signed the waiver. Of course you did.
Billy Gambino
The ontological rupture induced by somatic genome integration fundamentally destabilizes the homeostatic equilibrium of xenobiotic metabolism. The adenoviral and AAV vectors, while ostensibly inert delivery platforms, trigger cascades of innate immune activation that dysregulate hepatic CYP450 isoforms-particularly CYP3A4 and CYP2C9-thereby inducing pharmacokinetic drift that defies predictive modeling. The absence of longitudinal pharmacogenomic databases renders post-intervention drug management epistemologically untenable. We are not merely treating disease-we are reconfiguring human biochemistry without a control group.
Karen Werling
I work with families who’ve had gene therapy done. One mom told me her 7-year-old got the treatment and now she can’t take Tylenol without getting sick. They’re doing monthly blood tests, but no one gave them a printed list of what to avoid. I made a little cheat sheet with emojis-red X for bad meds, green check for safe ones. It helped so much. If anyone wants it, DM me. We need more of these simple tools 💙
STEVEN SHELLEY
THIS IS A GOVERNMENT BIO WEAPON. THEY’RE PUTTING VIRUSES IN YOU TO CONTROL YOUR METABOLISM SO THEY CAN MAKE YOU DEPENDENT ON THEIR DRUGS. THE FDA IS IN ON IT. THEY’RE USING THIS TO KILL PEOPLE WHO DON’T TAKE THEIR PRESCRIPTIONS. I KNOW A GUY WHO GOT IT AND HIS KID DIED FROM A ‘STOMACH ULCER’-THAT WASN’T AN ULCER, THAT WAS A TARGETED TOXIN. CHECK YOUR URINE. THEY’RE SHEDDING NANOBOTS. YOU THINK IBUPROFEN IS DANGEROUS? WAIT TILL YOU SEE WHAT’S IN YOUR SALIVA AFTER THE INJECTION. 🚨
Emil Tompkins
Oh wow. So now we’re supposed to believe that a one-time treatment that rewires your DNA is somehow safer than taking a pill every day? That’s not science. That’s a cult. And you’re all just sheep waiting for your next injection. Meanwhile, your kid’s getting exposed to your shedded virus at Thanksgiving dinner and nobody’s even talking about it. Brilliant. Just brilliant.
Kevin Stone
It’s irresponsible to suggest that patients should carry medical alert cards. Most people don’t even know what their own blood type is. This isn’t a solution-it’s a burden placed on the vulnerable. And yet the pharmaceutical companies profit while the system fails. You can’t just hand someone a 50-page pamphlet and say ‘be safe.’ That’s not care. That’s negligence dressed up as caution.
Natalie Eippert
Why are we letting foreign scientists develop these therapies? The FDA is too slow. We need American-made gene therapies with American oversight. No more relying on European labs or Asian data. This is a national security issue. Our children’s DNA should not be modified by overseas corporations with no loyalty to American families. We need a ban on all non-domestic vectors. Period.
kendall miles
Did you know that in New Zealand, they’ve banned all AAV therapies over 50% efficacy because of the long-term cancer risk? We’ve got data from 2021 that shows 1 in 12 patients developed clonal expansion within 4 years. But the US is too busy chasing profits to listen. You think you’re getting cured? You’re getting a ticking time bomb with a warranty.
Gary Fitsimmons
I’ve seen this firsthand. My sister got the therapy last year. She’s doing amazing-can run now, no more hospital stays. But the drug changes? Yeah, it messed with her blood pressure meds. Took three months to figure it out. The docs didn’t know either. Just kept saying ‘wait and see.’ So I kept a notebook. Every pill. Every symptom. Every weird feeling. That’s what saved her. Don’t wait. Write it down. Talk to your pharmacist. You’re not alone.