Newborn Medication Safety Checker
Medication Safety Assessment
Check if medications are safe for jaundiced newborns based on bilirubin levels, age, albumin, and G6PD status. Follows AAP 2023 guidelines for kernicterus prevention.
Enter values to check medication safety.
Why Some Medications Can Trigger Brain Damage in Newborns
Most parents assume that if a doctor prescribes a medication for their newborn, it’s safe. But in the case of sulfonamides and a few other drugs, that assumption can be deadly. Kernicterus - a rare but devastating form of brain damage caused by too much bilirubin in a baby’s blood - is almost always preventable. Yet every year, it still happens. And too often, it’s because a medication was given that shouldn’t have been.
Here’s the cold truth: giving sulfonamides to a jaundiced newborn isn’t just risky. It’s a known trigger for irreversible neurological injury. The baby’s brain turns yellow. Not from the skin - from bilirubin staining the deep nuclei that control movement, hearing, and even breathing. The damage is permanent. No surgery, no therapy can undo it.
What Is Kernicterus - And Why Does It Happen?
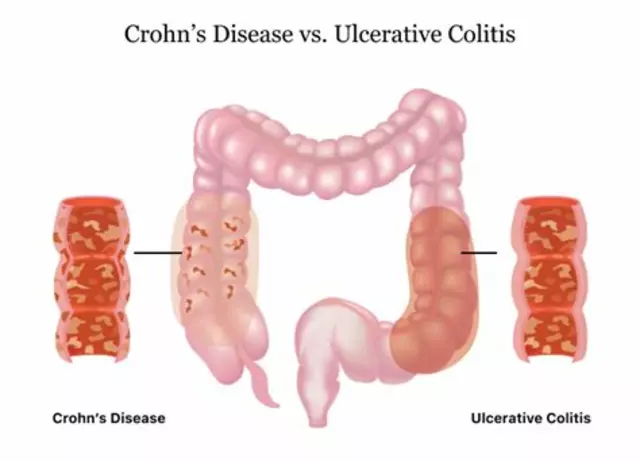
Kernicterus isn’t jaundice. Jaundice is common. It’s the yellow tint in a baby’s skin and eyes caused by bilirubin, a byproduct of normal red blood cell breakdown. In most cases, the liver clears it out. But in newborns, especially those under two weeks old, the liver is still learning how to do its job.
When bilirubin builds up too high - and stays there too long - it can cross the immature blood-brain barrier. Once inside the brain, it sticks to nerve cells and kills them. The result? Cerebral palsy, hearing loss, gaze problems, intellectual disabilities. Some babies die. Others live with lifelong disabilities.
According to a 2019 study of nearly a million Swedish infants, kernicterus affects about 1.3 in every 100,000 full-term newborns. That sounds rare. But here’s the kicker: 43% of those cases had no clear medical reason for the high bilirubin. That means the damage wasn’t unavoidable - it was missed, delayed, or triggered by something preventable.
How Sulfonamides Turn a Manageable Condition Into a Crisis
Bilirubin doesn’t float freely in the blood. It binds to albumin, a protein that carries it safely to the liver. Think of albumin as a taxi. Bilirubin hops in. The taxi drives it to the liver. No problem.
But some drugs - like sulfonamides - are like pickpockets. They sneak into the taxi, push bilirubin out, and leave it stranded. Suddenly, there’s too much free bilirubin in the blood. It doesn’t need to wait for the liver. It can slip right through the blood-brain barrier and into the brain.
Sulfisoxazole and sulfamethoxazole are the most common offenders. Studies show they can displace 25-30% of bilirubin from albumin at standard doses. That’s not a little bump. That’s enough to push a baby from safe to dangerous in hours.
The American Academy of Pediatrics (AAP) has labeled sulfonamides as high-risk since 2022. They don’t just say “be careful.” They say: Avoid them entirely when bilirubin levels are near treatment thresholds. That means if a baby’s bilirubin is at 75% of the phototherapy cutoff, sulfonamides are off the table.
Other Medications That Pose the Same Danger
Sulfonamides aren’t alone. Other drugs can do the same thing:
- Ceftriaxone - a common IV antibiotic - displaces 15-20% of bilirubin. It’s less risky than sulfonamides, but still dangerous in jaundiced infants.
- Aspirin and other salicylates - even baby aspirin - can displace bilirubin. Never give aspirin to a newborn.
- Furosemide - a diuretic sometimes used for fluid overload - can reduce albumin levels and increase free bilirubin.
And here’s something many clinicians miss: the risk isn’t just about the drug. It’s about the baby’s condition. If the baby has acidosis, low albumin (below 3.0 g/dL), or is premature, the risk skyrockets. A baby with 12 mg/dL bilirubin might be fine - unless they’re on sulfonamides and have an albumin level of 2.8.

Why G6PD Deficiency Makes Everything Worse
One in 14 babies globally has glucose-6-phosphate dehydrogenase (G6PD) deficiency. That’s about 7% of newborns. It’s more common in babies of African, Mediterranean, or Southeast Asian descent.
These babies break down red blood cells faster. More red cells = more bilirubin. Add a sulfonamide? That’s a perfect storm. Hemolysis spikes bilirubin. The drug pushes even more bilirubin out of albumin. The brain gets flooded.
There’s no excuse for giving sulfonamides to a baby with G6PD deficiency. Screening is simple, fast, and widely available. If you don’t know the status, assume the baby is at risk until proven otherwise.
Real Cases. Real Consequences.
A 5-day-old girl in Texas had a UTI. Her bilirubin was 14.2 mg/dL - high, but not yet at phototherapy threshold. She was given sulfisoxazole for prophylaxis. Twelve hours later, her bilirubin jumped to 22.7 mg/dL. She needed emergency phototherapy and nearly required an exchange transfusion.
A late preterm infant in Ohio received sulfamethoxazole-trimethoprim for suspected sepsis. His bilirubin was 13.5 mg/dL - “normal” for his age, according to some outdated charts. He developed kernicterus. He now has severe hearing loss and motor delays.
The Birth Injury Justice Center reviewed over 200 kernicterus cases. In 12% of them, the root cause was a sulfonamide given to a jaundiced baby. The average settlement? $4.2 million. That’s not just money. That’s a lifetime of care for a child who could have been protected.
How to Prevent This - Step by Step
Preventing medication-related kernicterus isn’t complicated. It’s about discipline.
- Check bilirubin levels before giving any drug. Don’t assume. Don’t guess. Test. If bilirubin is above 75% of the phototherapy threshold for that baby’s age in hours, avoid sulfonamides, ceftriaxone, and salicylates.
- Check albumin. If albumin is below 3.0 g/dL, the risk doubles. Use the bilirubin-albumin ratio. Healthy term infants: 0.5-1.0 mg bilirubin per gram of albumin. Below that, you’re in danger zone.
- Screen for G6PD deficiency. If the baby’s family background suggests risk, test. If you’re in a rush, treat as if they’re positive.
- Choose safer alternatives. Amoxicillin-clavulanate is just as effective for most infections and doesn’t displace bilirubin. It’s more expensive - about $2.50 per dose vs. $0.05 for sulfonamides - but it’s worth every penny.
- Use electronic alerts. Hospitals with automated EHR alerts that block sulfonamides when bilirubin is high have seen a 87% drop in medication-related kernicterus cases.
Many community hospitals still don’t have these alerts. If you’re in one, print out the AAP’s 5-step checklist. Tape it to the med cart. Make it part of every newborn’s med order.

The Bigger Picture: Why This Still Happens in 2025
Why do we still see these mistakes? Three reasons:
First, misconceptions about bilirubin. Some still think “if the bilirubin is under 15, it’s fine.” But bilirubin thresholds change by the hour. A level that’s safe at 24 hours isn’t safe at 72.
Second, resource gaps. In rural or low-income hospitals, rapid bilirubin testing isn’t available. That’s why the NIH launched a $2.4 million project in early 2023 to develop point-of-care free bilirubin devices. Until those arrive, use clinical judgment - and err on the side of caution.
Third, outdated habits. In some places, sulfonamides are still used because they’re cheap. But cost savings aren’t worth brain damage. The AAP and CDC both agree: safer alternatives exist for 92% of cases where sulfonamides were once used.
What’s Changing - And What’s Next
Good news: awareness is rising. In 2015, only 42% of U.S. hospitals had protocols to prevent medication-induced kernicterus. By 2023, that jumped to 78%. Epic Systems now automatically blocks sulfonamide orders in neonates with high bilirubin. The AAP’s 2023 guidelines include exact numerical thresholds for every age group.
The future? Real-time free bilirubin testing. AI-driven alerts in EHRs. Mandatory G6PD screening at birth in high-risk populations. These aren’t distant dreams - they’re already being rolled out in top pediatric centers.
But technology won’t fix everything. Only vigilance will. Every nurse, every doctor, every pharmacist needs to know: One wrong drug. One delayed test. One assumption. That’s all it takes.
Frequently Asked Questions
Can kernicterus be reversed if caught early?
No. Once bilirubin has entered the brain and caused damage, the injury is permanent. The only chance to prevent it is to stop the bilirubin from crossing the blood-brain barrier in the first place. That means early detection of jaundice, timely phototherapy, and avoiding drugs that displace bilirubin. There’s no cure after damage occurs.
Are all antibiotics dangerous for jaundiced newborns?
No. Only specific drugs that displace bilirubin from albumin are risky. Sulfonamides, ceftriaxone, and aspirin are the main culprits. Most common antibiotics - like amoxicillin, ampicillin, and cefazolin - are safe. Always check the drug’s bilirubin-displacing potential before giving it to a newborn with elevated bilirubin.
How do I know if my baby is at risk for G6PD deficiency?
G6PD deficiency is more common in babies of African, Mediterranean, Middle Eastern, or Southeast Asian descent. If your family comes from one of these regions, assume risk until tested. Screening is done with a simple heel prick blood test and takes less than 10 minutes. Many hospitals now screen all newborns in high-prevalence areas.
Is it safe to give sulfonamides to a newborn if bilirubin is normal?
Even if bilirubin is currently normal, it can spike rapidly. A baby’s bilirubin level can double in 12 hours. Sulfonamides can trigger that spike. The AAP recommends avoiding them entirely in infants under 2 months, regardless of current bilirubin levels. It’s not about today’s number - it’s about the potential for tomorrow’s crisis.
What should I do if my baby was given a sulfonamide and now looks more jaundiced?
Get immediate medical attention. Request a repeat bilirubin test - preferably a total and free bilirubin level - and ask for an albumin test. Do not wait. If bilirubin is rising quickly, phototherapy may be needed immediately. In severe cases, an exchange transfusion could be life-saving. Time is the enemy here.
What Comes Next
If you’re a parent: Ask your pediatrician, “Is this medication safe for a jaundiced baby?” Don’t be afraid to push. If you’re a clinician: Double-check every antibiotic order for a newborn. Use the checklist. Trust the data. If you’re in a hospital without protocols: Start building them. This isn’t about blame. It’s about stopping preventable harm.
Kernicterus doesn’t have to happen. Not today. Not tomorrow. Not ever again.



Suzan Wanjiru
I work in neonatal ICU and this is 100% true. Saw a baby go from 12 to 24 bilirubin in 8 hours after a simple UTI antibiotic. No one checked the med list. We got lucky with phototherapy but the parents still have nightmares. Always ask about meds before assuming they're safe.
And yes, sulfonamides are still prescribed in some rural clinics because they're cheap. That's not acceptable.
Kezia Katherine Lewis
The displacement mechanism of sulfonamides from albumin-bound bilirubin is a well-documented pharmacokinetic interaction. The free fraction of bilirubin increases exponentially when albumin binding sites are competitively inhibited, particularly in neonates with immature hepatic conjugation and low albumin concentrations. This is not theoretical-it’s a validated clinical phenomenon with clear biomarkers and therapeutic thresholds.
Henrik Stacke
I’ve seen this happen in the UK too. A baby in our unit got ceftriaxone for suspected sepsis-bilirubin was ‘only’ 14. Two days later, he was having seizures. The parents didn’t even know what bilirubin was. We lost so much time because no one thought to question the antibiotic. It’s not just about the drug-it’s about culture. We need to stop treating neonates like tiny adults. One wrong pill. One missed check. One assumption. And it’s over.
Manjistha Roy
I’m from India, and G6PD deficiency is incredibly common here-nearly 1 in 8 boys. We screen all newborns in our region now, and it’s saved lives. But many private hospitals still skip it because it’s ‘not standard.’ This isn’t just about meds-it’s about equity. If your baby is from a high-risk background, and you’re not tested, you’re being set up to fail. Please, hospitals: make G6PD screening mandatory, not optional.
Jennifer Skolney
I’m a mom of a preemie who had jaundice. We were given sulfamethoxazole because the doctor said it was ‘standard.’ I didn’t know any better. My baby’s bilirubin spiked. We had to do phototherapy for 72 hours. I cried for days. Please, if you’re a parent-ask. Ask. ASK. Don’t trust the system. Trust your gut. And if something feels off-push harder. I wish I had.
❤️
JD Mette
The AAP guidelines are clear. The data is solid. The consequences are irreversible. Yet we still see this happen. It’s not malice. It’s complacency. Busy shifts. Outdated protocols. Assumptions that someone else checked. We need systems-not just reminders. Automated alerts. Mandatory checks. No exceptions. Because when it’s your baby, there’s no second chance.
Olanrewaju Jeph
In Nigeria, we lack resources but not knowledge. Our pediatricians know the risks. The problem is access to rapid bilirubin tests and alternatives. Many use sulfonamides because amoxicillin is out of stock. This is not negligence-it’s systemic failure. We need international support for point-of-care bilirubin devices. Not just guidelines. Tools. Funding. Logistics. Otherwise, the same babies keep paying the price.
Kane Ren
I used to think jaundice was just a yellow baby. Then my nephew got kernicterus after a simple ear infection antibiotic. He’s 6 now. Can’t walk right. Can’t hear his own name. We were told it was ‘bad luck.’ But it wasn’t. It was a missed check. A wrong pill. A system that didn’t care enough to ask. I’m not angry. I’m just done pretending this is rare. It’s not. It’s preventable. And that’s the worst part.
Charmaine Barcelon
This is why I hate when people say ‘trust your doctor.’ Your doctor didn’t go to medical school to kill babies. But they’re tired. Overworked. And they still use old protocols. I’ve seen nurses give sulfonamides to jaundiced babies and say ‘it’s fine, he’s not that yellow.’ NO. IT’S NOT FINE. YOU’RE NOT A DOCTOR. YOU’RE A NURSE. CHECK THE BILIRUBIN. CHECK THE ALBUMIN. CHECK THE MEDS. OR YOU’RE PART OF THE PROBLEM.
Karla Morales
The real scandal? This isn’t even about the drugs. It’s about the $$$ 💸. Sulfonamides cost $0.05. Amoxicillin? $2.50. Hospitals save $200K a year by using cheap antibiotics. And who pays? The child. The family. The taxpayer in lifelong care. This isn’t medical negligence. It’s corporate greed wrapped in a white coat. The AAP guidelines? Ignored. The EHR alerts? Turned off. The babies? Forgotten. 💔