Bacterial vaginosis: symptoms, treatment, and prevention
Bacterial vaginosis (BV) happens when the normal balance of bacteria in the vagina shifts. Most people notice a thin, gray or white discharge and a fishy smell that gets stronger after sex. Some have mild burning or itching; others feel nothing. BV isn’t a yeast infection — it needs a different approach.
Symptoms and diagnosis
Don’t guess. If your discharge changes or you notice a strong odor, see a clinician. Diagnosis is usually quick: your provider will ask about symptoms, do a pelvic exam, and test a sample of vaginal fluid. Labs check pH and the mix of bacteria. Common checks include Amsel’s criteria and sometimes a Gram stain called the Nugent score. Getting it right matters because the wrong treatment won’t help and symptoms can come back.
BV raises the chance of getting or spreading STIs and, if you’re pregnant, can increase the risk of preterm birth. If you have more than three episodes in a year, that’s called recurrent BV and deserves a focused plan with your clinician.
Treatment and prevention
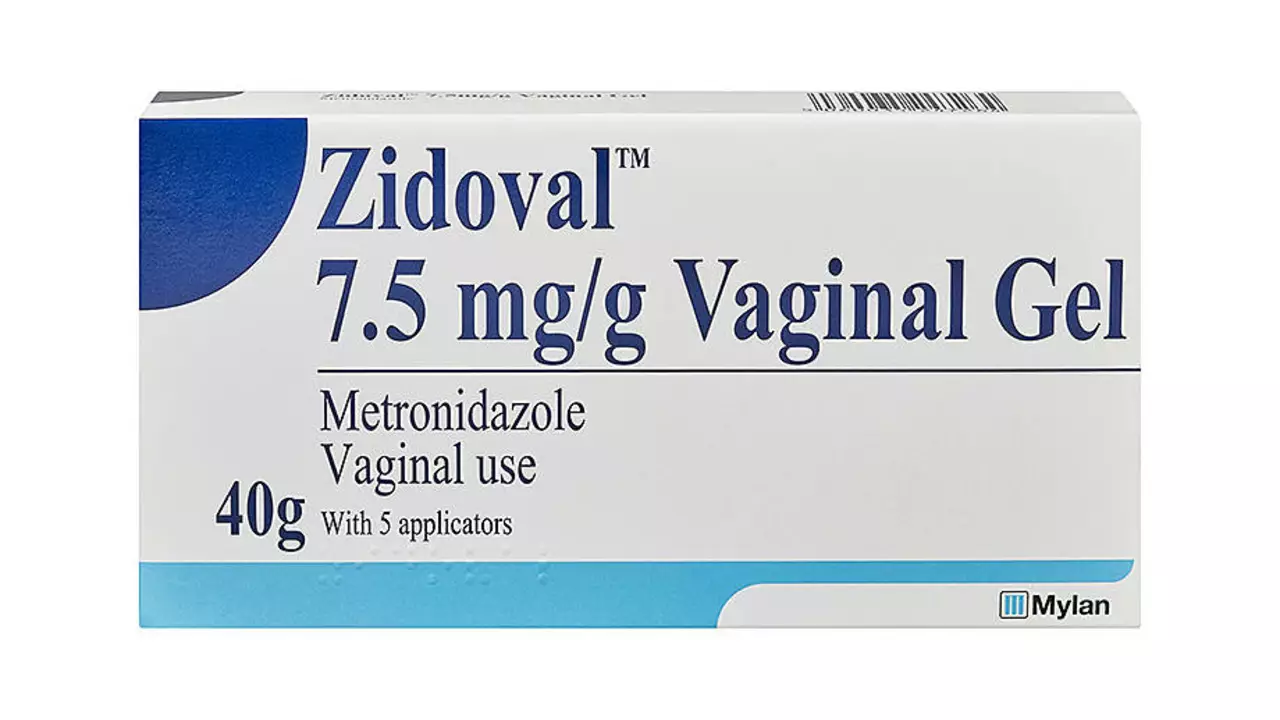
First-line treatments are metronidazole (oral or gel) or clindamycin cream. Most people feel better in a few days, but finish the full course to reduce relapse risk. Avoid alcohol during and 24 hours after metronidazole. If symptoms return quickly after treatment, tell your provider — they may switch meds or recommend longer, low-dose maintenance therapy.
Simple daily habits help prevent BV. Don’t douche. Avoid scented washes, strong soaps, and fragranced tampons, which disrupt the natural flora. Use condoms consistently — semen can change vaginal pH. Limiting new or multiple partners also reduces risk. Some people try probiotics with Lactobacillus strains; evidence is mixed, but some find benefit. Talk with your clinician before starting supplements.
For persistent BV, options can include a longer oral antibiotic course, twice-weekly topical treatment for several months, or referral for specialist care. Some clinics offer testing to rule out other infections or to check for resistant bacteria. Home remedies like plain yogurt applied topically are common myths — they won’t replace medical treatment and can sometimes cause irritation.
When to seek urgent care: if you have fever, severe pelvic pain, heavy unusual bleeding, or are pregnant and notice any symptoms. Otherwise, make an appointment when symptoms start so treatment can be started quickly. Keep a short record of triggers — new soap, recent antibiotics, or changes in partners — to help your clinician find patterns.
Need more detail on medications or local care options? Check a trusted health site or contact your healthcare provider for guidance tailored to your situation. Quick treatment lowers complications and helps you get back to normal faster.