Osteoporosis treatment: simple steps to lower fracture risk
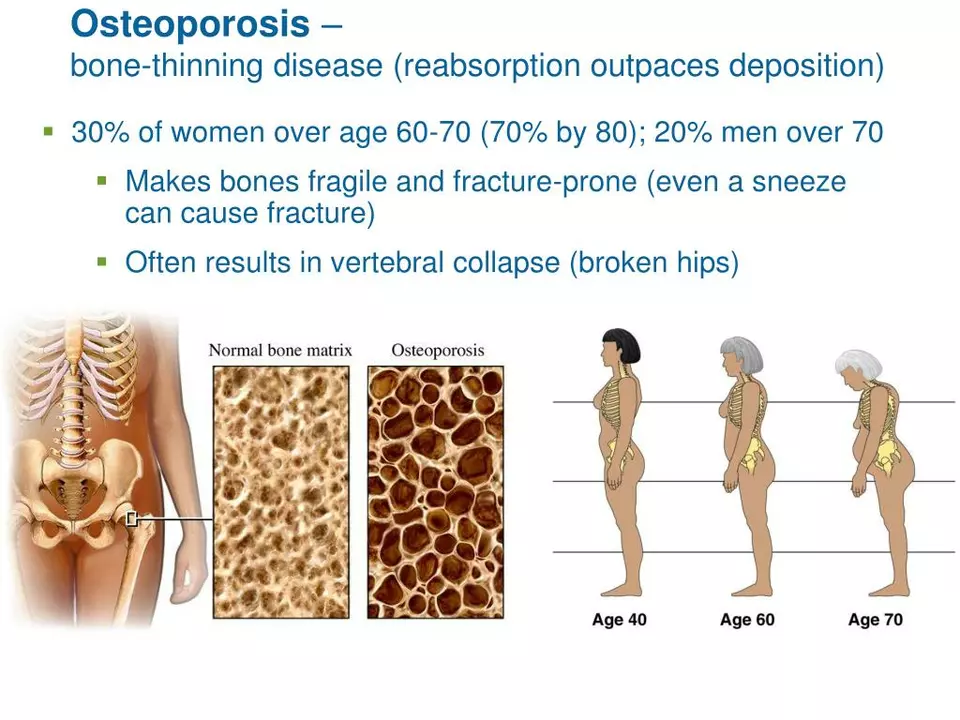
One in three women over 50 and one in five men will break a bone due to weak bones. If that sounds scary, know this: small, steady changes plus the right meds when needed cut your risk a lot. Start by finding out where you stand.
Get a DXA (bone density) scan and ask your doctor for a FRAX risk estimate. These tests tell you if you need treatment now or if lifestyle changes are enough. Bring a full list of medicines and health issues—some drugs, low thyroid function, or long steroid use raise bone loss risk and change the plan.
Quick, practical actions you can do today
Eat for bones: aim for about 1,000–1,200 mg of calcium daily from foods like milk, yogurt, sardines, tofu, and leafy greens. Check vitamin D with a 25‑hydroxy vitamin D blood test; many adults need supplements (often 800–2000 IU daily) to reach a safe level. Talk to your doctor before starting supplements if you have kidney issues.
Move smart: do weight‑bearing activities (walking, dancing, stair climbing) and two or more weekly strength sessions (squats, rows, light weights). Add balance work—tai chi or simple single‑leg stands—to cut fall risk. Aim for 20–40 minutes most days, and build up slowly.
Make your home safer: remove loose rugs, add night lights, secure handrails, and use non‑slip mats. Review any medicines that cause drowsiness or low blood pressure with your clinician. Quit smoking and keep alcohol to low levels—both harm bone quality and increase falls.
Medications: what they do and what to expect
Bisphosphonates (alendronate, risedronate, zoledronic acid) slow bone loss and cut spine and hip fractures. They’re common first choices. Take oral forms as directed to avoid reflux; IV options work if pills are a problem. Doctors often reassess after 3–5 years to consider a “drug holiday” for some patients.
Denosumab is a twice‑yearly injection that lowers fracture risk strongly, but stopping it can cause quick bone loss. If you start it, plan the follow‑up with your doctor. Anabolic drugs (teriparatide, abaloparatide, romosozumab) build new bone and are used for severe osteoporosis or after fractures; they’re usually time‑limited and require monitoring.
Expect regular follow up: repeat DXA scans every 1–2 years in many cases, plus blood tests for calcium and kidney function when needed. Get a dental check before some treatments and report new thigh pain or jaw soreness right away.
Ask clear questions: what is my 10‑year fracture risk, what are the likely benefits of this treatment for me, what side effects should I watch for, and how will we know it’s working? With tests, daily habits, home safety fixes, and the right meds when needed, most people cut fracture risk and keep living active lives.