HIV Protease Inhibitor Comparison Tool
Compare HIV Protease Inhibitors
Select two drugs to compare their key characteristics and make an informed decision about treatment options.
When you or a loved one needs to keep HIV under control, the choice of protease inhibitor can feel like a gamble. Indinavir is a once‑daily pill that’s been around since the late 1990s, but newer agents promise fewer side effects and smoother dosing. This guide breaks down the hard facts so you can decide whether Indinavir still makes sense or if a newer alternative is a better fit for your lifestyle and health goals.
Key Takeaways
- Indinavir is effective but carries a high risk of kidney stones and requires careful hydration.
- Saquinavir and Lopinavir/ritonavir are older drugs with similar efficacy but more gastrointestinal issues.
- Atazanavir and Darunavir provide once‑daily dosing with fewer metabolic problems.
- Ritonavir is rarely used alone; it boosts the levels of other protease inhibitors.
- Cost, pill burden, and individual kidney or liver health are the top three decision factors.
What makes a protease inhibitor work?
All protease inhibitors target the HIV‑1 protease enzyme, preventing the virus from maturing into its infectious form. By blocking this step, they dramatically lower viral load and allow the immune system (measured by CD4 count) to rebound. The class shares a core mechanism, but small differences in chemistry create distinct absorption, metabolism, and side‑effect profiles.
How Indinavir stacks up
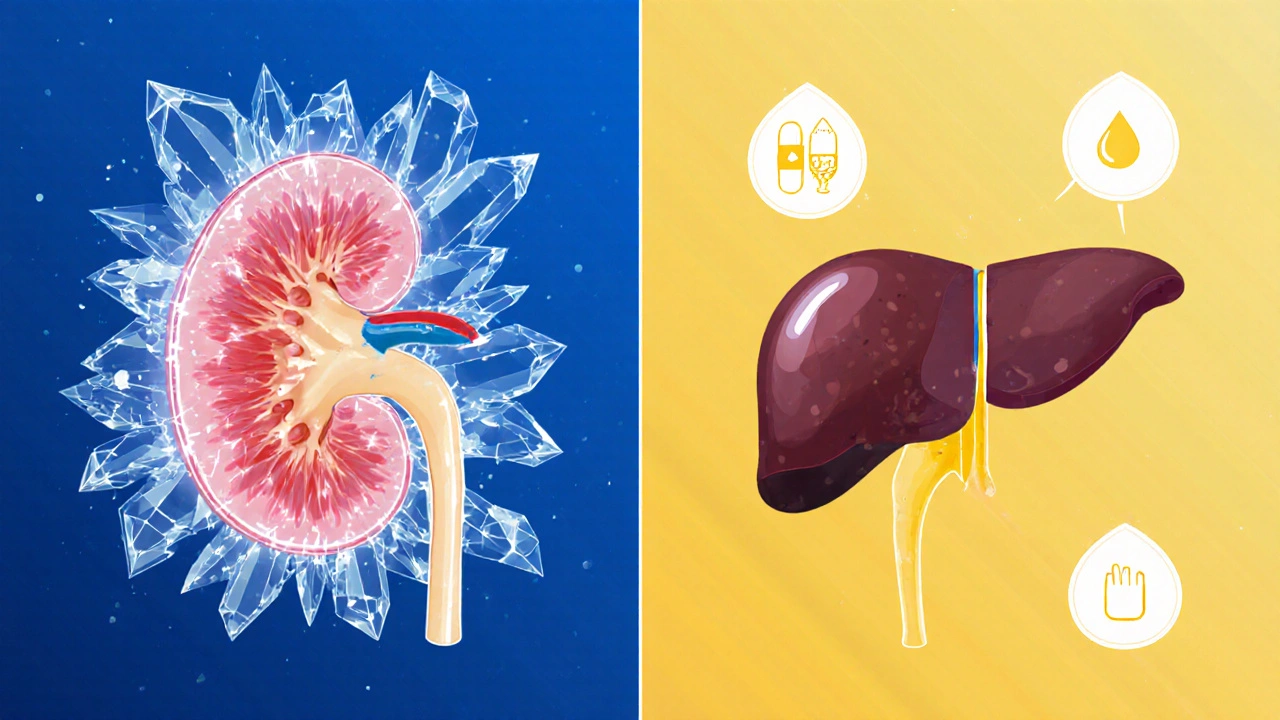
Indinavir (trade name Crixivan) is a protease inhibitor that was approved in 1997 and quickly became a staple of early HAART regimens. Its strengths are proven efficacy and a twice‑daily dosing schedule that fits many patients’ routines. However, it is notorious for:
- Kidney stone formation - up to 8% of users develop crystalluria.
- Hyperbilirubinemia - mild jaundice in about 5% of patients.
- Need for high fluid intake - at least 1.5L/day to dilute urine.
Because of these issues, clinicians often reserve Indinavir for patients with normal baseline renal function who can commit to the hydration regimen.
Alternatives worth a look
Below are the most common comparators, each defined once with schema markup.
Saquinavir an older protease inhibitor that requires a high‑fat meal for optimal absorption - still prescribed in resource‑limited settings.
Lopinavir/ritonavir a fixed‑dose combination (Kaletra) that pairs a potent inhibitor with ritonavir as a booster - commonly used in second‑line therapy.
Atazanavir a once‑daily inhibitor known for low lipid impact but a propensity for mild jaundice - favoured when metabolic health is a concern.
Darunavir the most potent newer protease inhibitor, usually given with ritonavir - the go‑to for patients with drug‑resistant virus.
Ritonavir originally a standalone drug, now primarily used at low doses to boost other protease inhibitors - essential for pharmacokinetic boosting.
Tipranavir a non‑peptidic inhibitor reserved for multi‑drug‑resistant cases - requires careful liver monitoring.
HIV the virus that causes AIDS, characterized by progressive immune system decline if untreated - the disease context that ties all these drugs together.
Side‑effect profile comparison
| Drug | Typical Dose | Frequency | Food Requirement | Key Side Effects | Renal Considerations | Average Monthly Cost (USD) |
|---|---|---|---|---|---|---|
| Indinavir | 800mg | Twice daily | None | Kidney stones, hyperbilirubinemia | High - hydrate ≥1.5L/day | ≈$150 |
| Saquinavir | 1000mg | Twice daily | High‑fat meal | Diarrhea, nausea | Low | ≈$120 |
| Lopinavir/ritonavir | 400/100mg | Twice daily | None | GI upset, lipid rise | Moderate | ≈$200 |
| Atazanavir | 300mg | Once daily | Empty stomach (no food 1h before/2h after) | Mild jaundice, low lipid impact | Low | ≈$210 |
| Darunavir (boosted) | 800mg + ritonavir 100mg | Once daily | None | Rash, lipid rise | Low | ≈$250 |
| Tipranavir (boosted) | 500mg + ritonavir 100mg | Twice daily | None | Liver toxicity, rash | Low | ≈$300 |
When to stick with Indinavir
If you’ve been stable on Indinavir for years, there’s no pressure to switch. The drug’s viral suppression rates (≈85% achieving <1000 copies/mL after 48 weeks) match many newer agents. Keep Indinavir if:
- You have normal kidney function (eGFR >90mL/min/1.73m²).
- You can reliably drink 2L of water daily.
- Your insurance covers it at a lower co‑pay than newer options.
- You have no history of nephrolithiasis.
Regular urine checks (every 3-6 months) help spot early crystal formation.
When a newer drug makes more sense
Switching is advisable if you notice any of these red flags:
- Frequent kidney stones or unexplained flank pain.
- Persistent mild jaundice that bothers you cosmetically.
- Difficulty adhering to a twice‑daily schedule.
- Emergence of drug‑resistant mutations in genotype testing.
In those cases, Atazanavir or Darunavir (both once‑daily) often restore convenience while keeping viral load suppressed.
Cost and access considerations in 2025
Generic Indinavir became available in 2022, dropping the monthly price to around $150 in the U.S. However, many insurers have shifted formularies toward newer generics, offering lower co‑pays for Atazanavir ($45) or Darunavir ($55). In Australia, the Pharmaceutical Benefits Scheme (PBS) lists Darunavir as a first‑line option for patients with high viral load, making it the most affordable choice for locals.
Putting it all together: decision flow
- Assess kidney health. If eGFR <60mL/min, avoid Indinavir.
- Check lifestyle: can you drink enough water? If not, pick a once‑daily agent.
- Review insurance formularies: compare out‑of‑pocket costs.
- Run a genotype test if viral load is rising; resistance may dictate a switch to Darunavir.
- Discuss with your clinician the need for a booster (ritonavir) - many newer drugs already come pre‑boosted.
Frequently Asked Questions
Can Indinavir cause permanent kidney damage?
Kidney stones are the main concern, but with proper hydration they rarely lead to lasting impairment. Regular monitoring and prompt stone management keep long‑term risk low.
Is a once‑daily regimen always better?
Convenience improves adherence, but the best choice balances dosing with side‑effect profile and drug interactions. For many patients, Atazanavir’s once‑daily schedule outweighs its mild jaundice risk.
Do I need a booster if I switch to Darunavir?
Yes, Darunavir is usually prescribed with low‑dose ritonavir (100mg) or cobicistat to reach therapeutic levels. Some formulations now include the booster in a single tablet.
How often should I get blood work while on these drugs?
Baseline labs (renal, hepatic, lipids) are taken before starting. After the first month, check renal function for Indinavir and liver enzymes for Tipranavir. Then every 3-6months for all protease inhibitors.
Is generic Indinavir as effective as the brand?
Regulatory agencies require bioequivalence, so generic Indinavir matches the brand’s viral suppression rates. The key differences lie in cost and packaging, not efficacy.
Next steps for you
Grab your latest lab results, note any kidney‑related symptoms, and bring them to your next HIV specialist appointment. Ask specifically about the cost‑share for Atazanavir or Darunavir on your plan - many clinics have patient‑assistance programs. If you decide to stay on Indinavir, set a daily water reminder and schedule a urine dip test every six months.
Remember, the goal is simple: keep the virus suppressed, stay healthy, and avoid side‑effects that derail your life. Whether you stick with Indinavir or switch to a newer option, a clear conversation with your care team will get you there.



khajohnsak Mankit
Reading through the protease inhibitor tableau feels like wandering a kaleidoscopic marketplace where each pill whispers a different promise-some echoing the clatter of vintage efficacy, others humming the soft lull of modern tolerability. The dance between renal vigilance and lipid serenity is not merely clinical; it’s a choreography of daily life, water bottles, and the occasional sigh of relief when the crystal‑free urine test comes back clean. In the grand tapestry of antiretroviral therapy, Indinavir remains a bold brushstroke, vivid yet edged with the risk of nephrolithiasis, demanding the patient’s devoted hydration ritual as a sacrament.
Jayant Paliwal
One must, with due deliberation, confront the manifold dimensions of protease inhibition; the landscape is not merely binary but replete with subtleties, contradictions, and paradoxes-each drug a chapter in a sprawling saga of pharmacologic evolution; the very act of selecting between Indinavir and its newer counterparts demands an appraisal of renal pharmacokinetics, hepatic metabolism, patient adherence patterns, and-perhaps most critically-the socioeconomic canvas upon which treatment unfolds. The hydrophilic demands of Indinavir, for instance, impose a quotidian ritual of fluid intake, a regimen that, while ostensibly simple, can become burdensome for those whose lifestyles are already fragmented by work, travel, and comorbidities. Conversely, agents such as Atazanavir or Darunavir proffer once‑daily dosing schemas, ameliorating the pill burden but introducing their own specters-jaundice in the former, lipid perturbations in the latter-each necessitating vigilant laboratory surveillance. Moreover, the economic vector cannot be ignored; generic Indinavir, despite its reduced price point, may be eclipsed by formulary preferences that privilege newer agents with lower co‑pays, thereby reshaping the cost‑benefit calculus in favor of what some might deem 'modern' therapy. The clinician, therefore, must wield a scalpel of precision, excising not only the pharmacologic inefficacies but also the psychosocial fissures that may precipitate non‑adherence. In sum, the decision matrix is an intricate mosaic-one that requires more than a cursory glance at dosing tables; it demands an empathic engagement with the patient’s narrative, a foresight into potential renal sequelae, and a strategic navigation of insurance formularies-lest the chosen regimen, however theoretically optimal, falters at the altar of real‑world implementation.
Kamal ALGhafri
From a pragmatic standpoint, the data clearly show that Indinavir's nephrotoxic profile is not a trivial side effect. Patients with baseline eGFR below 60 mL/min/1.73 m² should avoid it, as the incidence of crystal‑induced nephrolithiasis escalates dramatically. The newer agents provide comparable viral suppression with a more favorable safety margin.
Gulam Ahmed Khan
Hey folks! 🌟 If you’re still on Indinavir and managing the water intake, kudos to you! But if the stone‑forming saga feels like a nightmare, consider switching to a once‑daily option-your kidneys will thank you and you’ll have more time for the things you love. Keep pushing forward!
John and Maria Cristina Varano
Indinavir is old and pricey.
Melissa Trebouhansingh
While the discourse surrounding antiretroviral selection often gravitates toward simplistic cost analyses, it is imperative to recognize the nuanced interplay of pharmacodynamics and patient‑centred outcomes. The lexicon of “newer is better” neglects the oft‑overlooked adherence challenges posed by dietary stipulations, particularly with agents such as Saquinavir that necessitate high‑fat meals. Moreover, the ontological weight of renal considerations cannot be understated; indiscriminate prescribing of Indinavir without assessing baseline creatinine clearance may inadvertently precipitate iatrogenic nephrolithiasis. Hence, a holistic appraisal, integrating biochemical thresholds, socioeconomic variables, and lifestyle congruence, remains the cornerstone of optimal therapeutic orchestration.
Brian Rice
Upon rigorous examination of the comparative data, it becomes evident that the lipid‑raising potential of Lopinavir/ritonavir warrants careful monitoring, especially in patients with pre‑existing dyslipidemia. Conversely, Atazanavir’s propensity for mild hyperbilirubinemia, while cosmetically concerning, does not compromise virologic efficacy. The clinical decision should thus prioritize metabolic risk profiles alongside renal function.
Stan Oud
Honestly, the whole hype about newer PI’s is overrated; Indinavir still works if you drink enough water-simple math, no need for fancy boosters.
Ryan Moodley
In the grand theater of HIV treatment, the protagonists are not merely molecules but the narratives we craft around them; imagine the drama of a patient juggling twice‑daily dosing while the specter of kidney stones looms-a plot twist that only the seasoned antagonist, Darunavir, can thwart with its once‑daily charisma. The stakes are high, the side‑effects are the villains, and the clinicians, dear readers, are the directors shaping the ending.
carol messum
Indinavir works but you have to drink a lot of water. Newer pills are easier to take.
Jennifer Ramos
Great summary! 👍 If you’re weighing options, remember that insurance formularies often favor Atazanavir or Darunavir these days, making them more affordable than you might think. Keep an eye on side‑effect profiles as well.
Grover Walters
From an analytical perspective, the comparative efficacy metrics across protease inhibitors are remarkably consistent, yet patient‑specific variables such as renal clearance and pill burden remain decisive factors in regimen selection.
Amy Collins
The PK/PD interplay for each PI is crucial; for instance, Indinavir's crystal formation is a classic case of solubility‑driven toxicity.
amanda luize
While the mainstream narrative glorifies newer agents, one must question the hidden agendas-pharma incentives, insurance rebates, and the subtle erosion of patient autonomy under the guise of “advancement.” The color‑coded tables mask a deeper manipulation of prescriber behavior.
Chris Morgan
Switching from Indinavir to a once‑daily PI is a pragmatic step; the data support improved adherence and comparable virologic control.
Pallavi G
Absolutely, and to add a practical tip: for anyone staying on Indinavir, consider using a daily water‑tracking app to ensure you meet the 1.5‑L threshold. It’s a simple habit that can dramatically reduce stone formation risk.