INR Target Calculator
This calculator helps determine if your INR value falls within your therapeutic range based on your condition. Your target range varies depending on your specific medical condition. Enter your INR value and select your condition to see if it's within the ideal range.
Your INR Status:
INR 0.0Enter your INR value and select your condition to see results
Next Steps:
- Check the status above for your specific condition
When you're on a blood thinner like warfarin, your life changes in ways you might not expect. It's not just about popping a pill every day. It's about knowing your INR number - and what it really means for your body. This isn't just a lab result. It’s a daily balancing act between preventing clots and avoiding dangerous bleeding. And if you don’t understand it, you’re flying blind.
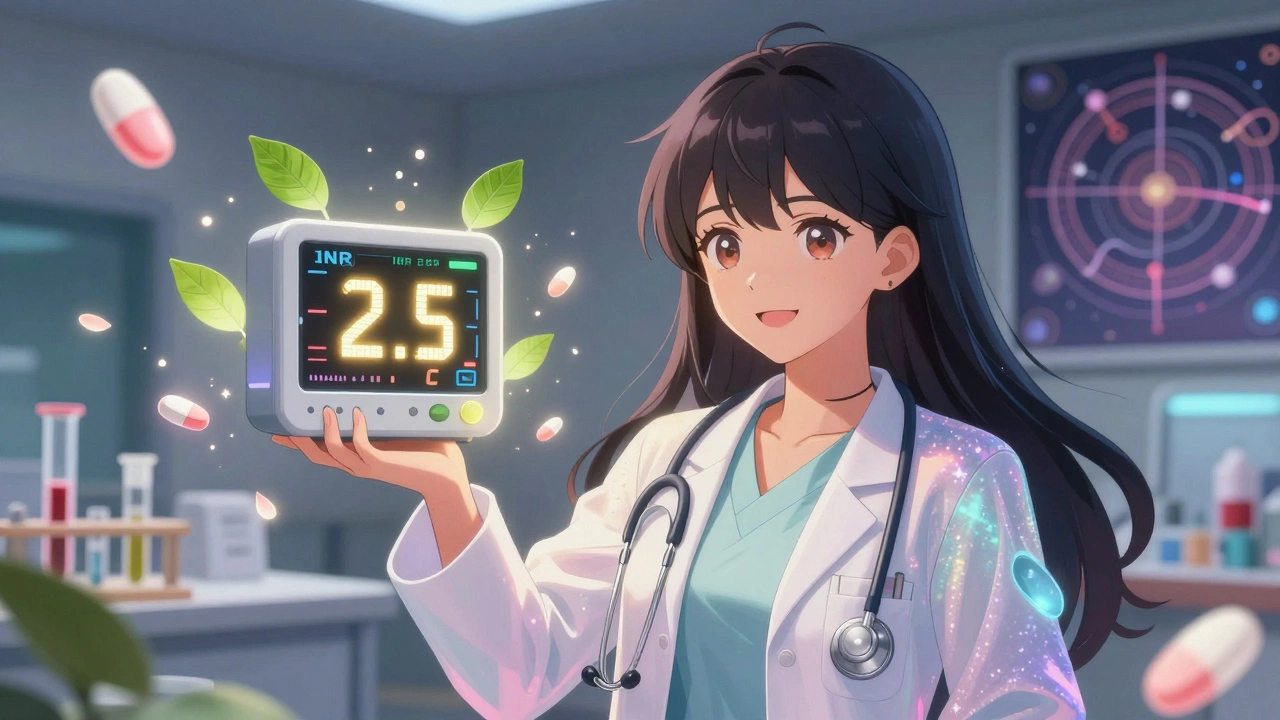
What Exactly Is INR?
INR stands for International Normalized Ratio. It’s a number that tells doctors how long it takes your blood to clot. Think of it like a speedometer for your blood’s clotting ability. A normal INR for someone not on blood thinners is 1.0. But if you’re taking warfarin, your target is usually between 2.0 and 3.0. That doesn’t mean you’re “thinner” - it means your blood takes a little longer to form clots, which is exactly what you want if you have atrial fibrillation, a mechanical heart valve, or a history of deep vein thrombosis.
The INR system was created in 1983 by the World Health Organization to fix a big problem: every lab used different reagents, so the same blood sample could give wildly different results. Now, no matter where you get tested - Melbourne, New York, or rural Queensland - a 2.5 INR means the same thing. That standardization cut medication errors by 35%, according to the American Society of Hematology.
Why Your Target INR Isn’t the Same as Everyone Else’s
Not everyone on warfarin has the same goal. Your target depends on your condition:
- Atrial fibrillation or DVT/PE: 2.0-3.0
- Mechanical aortic valve: 2.0-3.0
- Mechanical mitral valve: 2.5-3.5
Why the difference? A mitral valve is under more stress than an aortic one. It’s like comparing a car engine running at 3,000 RPM versus 1,500 RPM - you need more protection. Go too low, and you risk a stroke or clot. Go too high, and a simple bump could send you to the ER with internal bleeding.
Studies show that keeping your INR within 10% of your target reduces stroke risk by 60% in atrial fibrillation patients. But if your INR climbs above 4.9, your risk of major bleeding jumps 27% for every 0.5-point increase. That’s why a 5.2 INR isn’t just “a little high” - it’s a red flag.
How Often Should You Get Tested?
When you first start warfarin, you might need testing twice a week. Doses are being fine-tuned, your body is adjusting, and your liver is learning how to process it. Once you’re stable - meaning your INR stays within range for months - you can drop to once a month. But here’s the catch: 38% of patients are tested weekly even when they don’t need to, according to the American College of Physicians. That’s unnecessary stress, cost, and time.
Medicare and most private insurers cover monthly testing without copays if you’re stable. But if your INR fluctuates because you started a new antibiotic, changed your diet, or drank more alcohol, your doctor might ask you to test twice a week again. That’s not overkill - it’s smart.
Home Testing: Convenience vs. Complexity
Home INR monitors like the Abbott Acelis or Roche CoaguChek let you test with a single drop of blood from your finger. Results come in under a minute. No waiting for the lab. No scheduling. No sitting in a waiting room for an hour.
Patients who test at home spend 72% of their time in the therapeutic range - compared to 58% for those who go to clinics. That means 34% fewer clots and 21% fewer major bleeds. For someone with a mechanical valve, that’s life-changing.
But it’s not for everyone. About 25-30% of patients can’t use home devices because of shaky hands, poor eyesight, or memory issues. Elderly patients over 65 rate home testing at 3.1 out of 5 - compared to 4.3 for younger users. And if you miss the capillary tube on your finger, you waste a $6 test strip. One user on Reddit said, “After three years, I still miss the tube one in five tests.”
Cost-wise, the device runs about $299 upfront. Each strip is $5.99. Medicare covers 100% for eligible patients. Private insurance usually covers 80%, leaving you with 20% coinsurance - and some insurers make you jump through hoops to get approved. About 31% of users report initial claim denials.
What Happens When Your INR Is Off?
INR below 1.5? You’re at risk of a clot. This is rare on warfarin unless you missed doses or started taking vitamin K-rich foods like kale or spinach - which counteract the drug. If your INR drops this low, call your doctor immediately.
INR above 5.0? You’re in danger zone. Your blood is taking too long to clot. Even a minor fall could cause bleeding in your brain or gut. The standard advice: skip your next warfarin dose and contact your provider within 24 hours. If your INR hits 8 or higher, you might need vitamin K or even a blood transfusion.
And here’s something few people realize: your INR can swing based on when you test. The American Heart Association recommends testing between 8 AM and 12 PM, after fasting 4-6 hours. Eating, drinking alcohol, or testing at 8 PM can throw off your results. Consistency matters more than you think.
Warfarin vs. DOACs: The Real Choice
Since 2010, new blood thinners - apixaban, rivaroxaban, dabigatran - have taken over. They don’t need INR checks. You take them once or twice a day, and that’s it. They’re easier. Safer. More predictable.
But they’re not for everyone. If you have a mechanical heart valve, DOACs won’t work. They’re also risky if you have severe kidney disease. And while DOACs cost $550-$650 a month, warfarin runs about $4. That’s a 170x difference.
Today, warfarin still makes up 30% of anticoagulant prescriptions in the U.S. - and nearly all of those 200,000 patients with mechanical valves rely on it. For them, INR monitoring isn’t a nuisance - it’s survival.
What You Can Do Today
If you’re on warfarin, here’s your action list:
- Know your target INR. Write it down. Put it on your fridge.
- Test at the same time every day. Consistency beats perfection.
- Track your diet. Vitamin K in leafy greens, cranberry juice, and alcohol can throw off your INR. Keep it steady.
- Ask if home testing is right for you. If you’re stable, mobile, and have good vision - it’s worth exploring.
- Call your doctor if your INR is below 1.5 or above 5.0. Don’t wait.
- Don’t let insurance denials stop you. If you’re denied, ask your doctor to appeal. It works more often than you think.
There’s no magic trick. No app that replaces your brain. But with the right knowledge, you’re not just managing a number - you’re protecting your life.
What’s Next for INR Monitoring?
Technology is catching up. In January 2023, the FDA approved the first smartphone-connected INR device - the Bayer CoaguChek ProConnect. It automatically sends your results to your doctor. No manual entry. No missed appointments. In trials, it was 98.7% accurate.
AI tools like the INR Advisor platform are now predicting the right warfarin dose with 83% accuracy, based on your history, diet, and meds. That’s not science fiction - it’s here.
But here’s the problem: rural areas still lag behind. Only 35% of rural clinics offer full anticoagulation management. Urban centers? 82%. That gap could mean the difference between a stroke and a second chance.
As DOACs grow - they’re expected to make up 85% of new prescriptions by 2028 - INR monitoring will become rarer. But for those who need it, it’s not going away. Not yet.
What does an INR of 2.5 mean?
An INR of 2.5 means your blood takes 2.5 times longer to clot than a person not on blood thinners. For most people on warfarin - like those with atrial fibrillation or a blood clot - this is the ideal middle of the target range (2.0-3.0). It balances the risk of clots and bleeding. It’s not too high, not too low. Just right.
Can I check my INR at home?
Yes, if you’re stable and your doctor approves. Home INR monitors like the Abbott Acelis or Roche CoaguChek use a tiny drop of blood from your finger and give results in under a minute. Medicare and many insurers cover them. But you need good eyesight, steady hands, and the ability to follow instructions. If you have arthritis, tremors, or dementia, home testing may not be safe.
Why does my INR change even if I take the same dose?
Warfarin is affected by many things: diet (especially vitamin K from greens), alcohol, antibiotics, even herbal supplements like garlic or ginkgo. Your liver’s ability to process it changes with illness, stress, or age. That’s why your dose isn’t set in stone - it’s adjusted based on your INR results, not your calendar.
What happens if I miss a warfarin dose?
If you miss one dose, take it as soon as you remember - but only if it’s the same day. Don’t double up the next day. If you miss more than one, call your doctor. Missing doses can drop your INR and increase clot risk. If you’re unsure, always check your INR before continuing.
Is INR monitoring necessary forever?
It depends on why you’re on warfarin. If you had a one-time blood clot and your doctor says you can stop after 3-6 months, you’ll stop testing. But if you have a mechanical heart valve, atrial fibrillation, or a genetic clotting disorder, you’ll likely need INR checks for life. Your condition, not your age, determines that.
Can I drink alcohol while on warfarin?
Moderate alcohol - one drink a day - is usually fine. But heavy drinking can spike your INR and raise bleeding risk. Binge drinking is dangerous. Alcohol also affects how your liver processes warfarin, so consistency matters. If you drink, keep it regular. Don’t save it all for weekends.




Geraldine Trainer-Cooper
INR isn't a number. It's a conversation your blood has with your liver every damn day.
Some days it's polite. Some days it screams.
You don't control it. You just learn to listen.
And yeah, that's terrifying.
But also kinda beautiful in a fucked-up way.
Kenny Pakade
Why are we still using 1980s tech when we have AI and smartphones?
Warfarin is a relic. Like fax machines for your blood.
And don't get me started on Medicare bureaucracy - it's worse than the CDC.
Brooke Evers
I just want to say how much I appreciate this post - I’ve been on warfarin for eight years after my pulmonary embolism, and honestly? Most people don’t get it.
You’re not just taking a pill. You’re managing a silent, ticking thing inside you.
It’s the diet changes - suddenly kale is your enemy.
It’s the anxiety every time you prick your finger.
It’s the guilt when you forget to test and your INR spikes.
It’s the loneliness when your friends say ‘just take the pill’ like it’s Advil.
I used to hate home testing because I’d cry over missed tubes.
Now I see it as my daily ritual - a tiny act of rebellion against chaos.
And when my INR hits 2.5? I feel like I won the lottery.
It’s not perfect.
But it’s mine.
And I’m still here.
So thank you for writing this.
Someone needed to say it.
Nigel ntini
The standardization of INR by the WHO in 1983 remains one of the most underappreciated public health achievements in hematology.
Before this, inter-lab variability led to catastrophic dosing errors - particularly in elderly patients with polypharmacy.
Modern DOACs offer convenience, but they lack the reversibility profile of vitamin K and fresh frozen plasma.
For patients with mechanical valves - especially those in resource-limited settings - INR monitoring is not merely advisable; it is indispensable.
Moreover, the cost differential between warfarin and DOACs is not trivial in low- and middle-income countries.
Let us not discard a proven, affordable tool in the name of novelty.
Ashish Vazirani
I'm from India, and here? We don't have home monitors. We wait. We drive. We pay. We cry. We wait again. And then? The doctor says, 'Oh, your INR is 5.2 - you need to stop warfarin for two days.' Two days?! What if I clot in the meantime? Who cares? The hospital is 80km away. No ambulance. No insurance. No help. Just a nurse who says, 'Try again next week.' This isn't healthcare. It's a lottery. And I'm losing.
Mansi Bansal
It is imperative to underscore the profound clinical implications of INR fluctuation, particularly in the context of pharmacokinetic variability induced by dietary vitamin K intake, concomitant antibiotic administration, and hepatic metabolic perturbations.
Furthermore, the assertion that home monitoring reduces bleeding events by 21% is statistically significant (p < 0.01) in multiple cohort studies, including the RIETE registry and the OUTPATIENT trial.
Nonetheless, the socioeconomic disparities in access to such technology remain an ethical imperative for policy reform.
It is not merely a medical issue - it is a matter of distributive justice.
Kay Jolie
Okay but have you considered the epistemology of INR?
It’s not just a number - it’s a metaphysical negotiation between your body and the pharmaceutical industrial complex.
Warfarin is the original biohack.
And home testing? That’s your personal data sovereignty in action.
You’re not just managing clotting - you’re reclaiming agency from the algorithmic healthcare machine.
Also, vitamin K is basically the anti-magic bullet.
And the CoaguChek ProConnect? That’s the future. We’re all cyborgs now.
Just saying.
pallavi khushwani
I think about INR like a quiet conversation with my own body.
It doesn’t shout. It whispers.
And if you’re not listening - really listening - it’ll slip away.
It’s not about being perfect.
It’s about showing up.
Every day.
Even when you’re tired.
Even when you hate the finger prick.
Even when the strip costs more than your coffee.
It’s not just medicine.
It’s a promise you make to yourself.
That you’ll keep living.
Even if it’s messy.
Even if it’s hard.
Even if no one else understands.
Dan Cole
Let’s be clear: DOACs are not superior - they’re just marketed better.
Warfarin has 40 years of real-world data. DOACs? 12.
And you think your fancy app is going to replace the human clinician who’s seen 500 INR curves?
That’s arrogance wrapped in Silicon Valley jargon.
Also, vitamin K isn’t ‘a dietary variable’ - it’s a biological constant.
And if you think a smartphone device is going to fix rural healthcare gaps, you’ve never been to West Virginia.
Stop romanticizing tech. Fix the system.
And for God’s sake, stop telling patients to ‘just test more.’
Some of us are working three jobs.
Billy Schimmel
So you’re telling me I need to prick my finger every week… for the rest of my life… to avoid a stroke?
And the cost of strips is more than my Uber eats?
And if I miss one, I’m a dead man walking?
Yeah.
Thanks for the pep talk, doc.
Love the optimism.
Shayne Smith
Just had my INR done today - 2.4. Felt like I won the lottery.
Also, I ate a salad. No drama. Just a salad.
And I didn’t cry.
Progress.
Jackie Petersen
Who owns the data from your home INR monitor?
Is it the device company?
The insurer?
The government?
What if they use it to raise your premiums?
What if they flag you as ‘high risk’ and deny your life insurance?
They’re watching. Always.
And they’re not your friend.
Warfarin isn’t medicine - it’s surveillance with a needle.
Annie Gardiner
Wait - so you’re saying INR is the only thing keeping me alive?
But what if I don’t want to be alive?
What if I’m tired?
What if the constant fear, the finger pricks, the diet police, the insurance denials - what if it’s just too much?
And now you want me to feel grateful?
That’s not empowerment.
That’s gaslighting with a lab report.