Crohn's disease: practical guide for everyday management
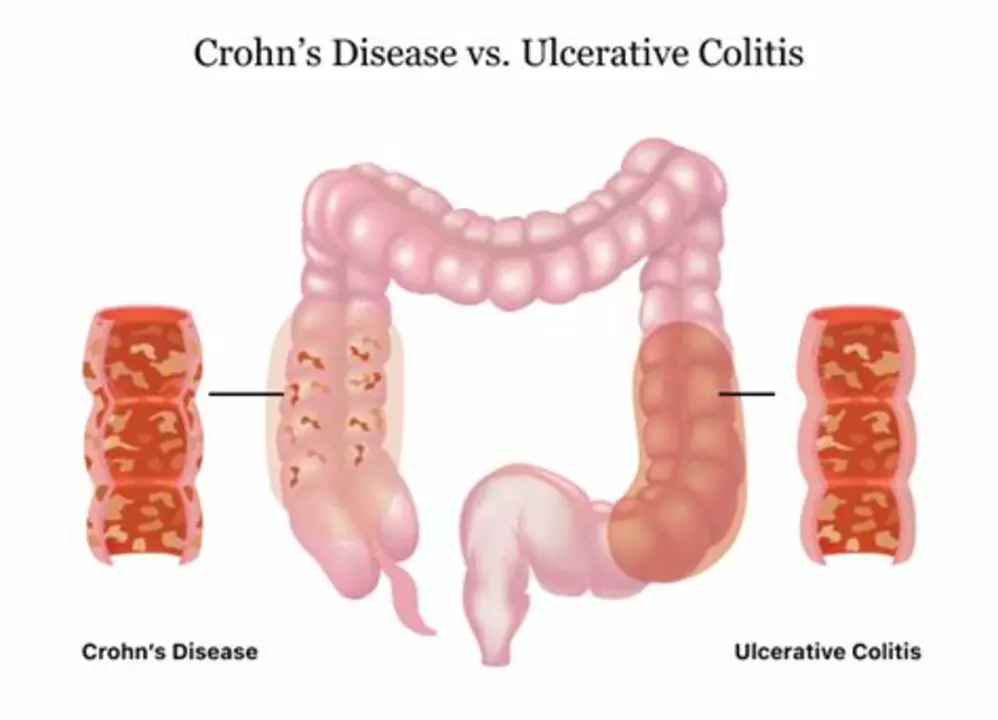
Crohn's disease is a long-term inflammatory bowel condition that can hit any part of the digestive tract. It causes belly pain, diarrhea, fatigue, and weight loss, but symptoms vary by person.
Symptoms and diagnosis
Typical symptoms include abdominal pain, diarrhea, an urgent need to go, blood in the stool, fever, weight loss, mouth sores, joint pain, and skin problems. If symptoms are sudden or severe, seek care.
How doctors diagnose Crohn's disease: stool tests to rule out infection, blood tests for inflammation and anemia, and colonoscopy with biopsies which is the main test. CT or MRI enterography shows small bowel disease. Diagnosis often needs repeat tests and specialist time.
Treatment and daily management
Treatments aim to reduce inflammation, control symptoms, and keep you in remission. Mild cases may get aminosalicylates or budesonide. Moderate to severe cases often need steroids for flares, then steroid-sparing options like immunomodulators such as azathioprine or 6-MP, or biologic drugs (anti-TNF, anti-integrin, anti-IL12/23).
Biologics like infliximab, adalimumab, vedolizumab and newer options work well for many people. Treatment choice depends on disease location, severity, prior meds, and side effects. Talk with your gastroenterologist about risks and monitoring.
Surgery is not a failure. It removes damaged bowel, treats strictures or fistulas, and can improve quality of life. Many people still need medicine after surgery to prevent recurrence.
Diet and lifestyle matter. No single Crohn's diet fits everyone. Keep a food diary to spot triggers like high-fiber raw vegetables, nuts, or dairy if you're lactose intolerant. During flares, low-residue meals and smaller portions help. Stay hydrated and consider a dietitian who knows IBD.
Managing flares: act fast. If your usual meds stop working or symptoms get worse, contact your care team. Short steroid courses, IV treatments, or hospitalization may be needed for severe flares. Monitor symptoms like high fever, severe pain, vomiting, or heavy bleeding — these need urgent care.
Practical daily tips: schedule medications, set refill reminders, join a local IBD support group or online community, and keep a list of current meds and allergy info. Mental health matters — anxiety and depression are common, so consider counseling when needed.
When to see a doctor: new persistent belly pain, unexplained weight loss, blood in stool, fever with symptoms, or signs of dehydration. For known Crohn's, worsening symptoms despite treatment, or new joint, eye, or skin problems.
You can live well with Crohn's. With clear communication with your gastroenterologist, a tailored treatment plan, and helpful daily habits, most people control symptoms and keep active.
Extra tips: get vaccinated for flu and COVID, talk about bone health if you use steroids, and avoid smoking — smoking makes Crohn's worse. Keep records of tests and endoscopy dates so you know when follow-ups are due. If you're planning pregnancy, discuss timing and meds with your doctor; many treatments can be adjusted safely. Always carry a doctor note for urgent care visits. Ask about clinical trials if standard options have failed; new therapies may help today.